Document Type : Original Research Article
Authors
- Valensa Yosephi 1
- Peter Yustian Atmaja 2
- Arif Nur Muhammad Ansori 3, 4, 5
- Ahmad Affan Ali Murtadlo 5, 6
- Viol Dhea Kharisma 5, 6
- Putu Angga Wiradana 7
- I Gede Widhiantara 7
- Sukma Sahadewa 8
- Maksim Rebezov 9
- Nikolai Maksimiuk 10
- Evgeniy Kolesnik 11
- Marina Derkho 12
- Natalia Koriagina 13
- Aswin Rafif Khairullah 14
- Fara Disa Durry 15
- Rahadian Zainul 16, 17
1 Master Program of Immunology, Postgraduate School, Universitas Airlangga, Surabaya, Indonesia
2 Department of Neurosurgery, dr. Moewardi General Hospital, Surakarta, Indonesia
3 Postgraduate School, Universitas Airlangga, Surabaya, Indonesia
4 Uttaranchal Institute of Pharmaceutical Sciences, Uttaranchal University, Surabaya, Indonesia
5 Department of Research and Development, Jalan Tengah, Surabaya, Indonesia
6 Faculty of Science and Technology, Universitas Airlangga, Surabaya, Indonesia
7 Research Group of Biological Health, Study Program of Biology, Faculty of Health and Science, Universitas Dhyana Pura, Bali, Indonesia
8 Faculty of Medicine, Universitas Wijaya Kusuma Surabaya, Surabaya, Indonesia
9 V.M. Gorbatov Federal Scientific Center for Food Systems of the Russian Academy of Sciences, Moscow, Russian Federation
10 The Institute of Medical Education, Yaroslav-the-Wise Novgorod State University, Velikiy Novgorod, Russian Federation
11 Department of Physiology, Ethology and Biochemistry of Animals, Russian State Agrarian University – Moscow Agricultural Academy named after K.A. Timiryazev, Moscow, Russian Federation
12 Department of Natural Sciences, South Ural State Agrarian University, Troitsk, Russian Federation
13 E.A. Vagner Perm State Medical University, Perm Krai, Russian Federation
14 Faculty of Veterinary Medicine, Universitas Airlangga, Surabaya, Indonesia
15 Faculty of Medicine, Faculty of Medicine, Universitas Pembangunan Nasional “Veteran” Jawa Timur, Surabaya, Indonesia
16 Department of Chemistry, Faculty of Mathematics and Natural Sciences, Universitas Negeri Padang, Padang, Indonesia
17 Center for Advanced Material Processing, Artificial Intelligence and Biophysics Informatics (CAMPBIOTICS), Universitas Negeri Padang, Padang, Indonesia
Abstract
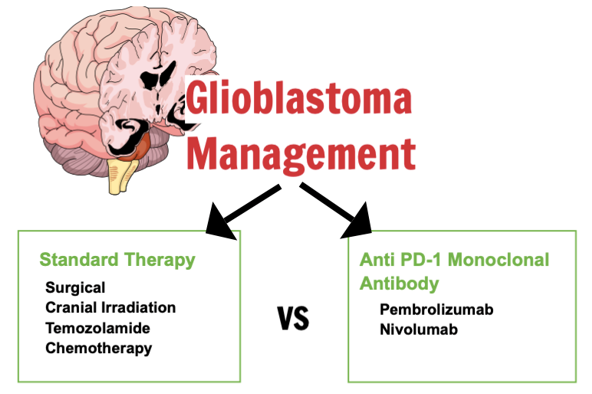
Monoclonal antibodies composed entirely of human immunoglobulin G4 that specifically target programmed death-1 (PD-1) are referred to as Nivolumab and Pembrolizumab. Monoclonal antibody of anti-PD-1 type for glioblastoma was found to be beneficial and harmless in preclinical research. Monoclonal antibody of anti-PD-1 (Pembrolizumab, Nivolumab) versus standard therapy for glioblastoma was systematically compared in terms of overall survival (OS), progression-free survival (PFS), and adverse events (AE). Pubmed, Scopus, Cochrane, and Clinicaltrials.gov databases were systematically searched through May 2023 for phase I or later RCTs reporting outcomes of interest. Inclusion RCTs criteria are adult population (>18 years old) with newly diagnosed or recurring cases of glioblastoma and have received immunotherapy with PD-1 inhibitors or standard treatment. For both OS and PFS, pooled effects estimates were computed using the approach of Cox proportional hazards regression. A computation was conducted on RCTs comprising 1680 patients from 4 included studies. Comparing anti-PD-1 monoclonal antibody to standard therapy, neither PFS nor OS improved at the median (HR = 1.08, 95% CI = 0.87-1.34, P = 0.51; P = 0.29; P = 0.29; and P = 0.29, 95% CI = 0.85-1.74, respectively). Furthermore, neither methylated nor un-methylated MGMT status benefits from anti-PD-1 monoclonal antibody (HR = 1.06, 95% CI = 0.89-1.27, P = 0.49; and HR = 1.29, 95% CI = 1.10-1.53, P = 0.002, respectively) in terms of overall survival. The anti-PD-1 antibody group experienced a greater incidence of AE (RR = 1.03, 95% CI = 0.94-1.14, P = 2.51). Anti-PD-1 monoclonal antibody did not demonstrate any clinical advantage over standard treatment for glioblastoma, according to this meta-analysis of four RCTs.
Graphical Abstract
Keywords
Main Subjects
Introduction
In adults, glioblastoma is the utmost prevalent malignant brain tumor [1,2]. The prevailing treatment approach presently comprises tumor excision via surgical means, succeeded by cranial irradiation and temozolomide chemotherapy [2,3].
Nevertheless, the conventional treatment for persons suffering from glioblastoma fails to enhance survival rates or prevent the recurrence of glioblastoma [4], underscoring the necessity for a novel therapeutic approach. Only 5% survive more than 5 years when given the standard-of-care [5]. One of the main reasons for this treatment failure is the resistance to temozolomide and the non-responding treatment process in cases (more than 50%) [6-8].
Studying immunotherapy to boost the immune response against tumors is crucial for treating glioblastoma as it offers a new approach. Recent research indicates that combination approaches, including as immune checkpoint inhibition and vaccinations, that target many arms of the cancer immune cycle, have demonstrated promise in preclinical models, and even in population of patients in other tumors [9-11].
Immune checkpoint inhibition shows promise as a potential therapy for glioblastoma [3]. It has been discovered that gliomas produce programmed death ligand-1 (PD-L1), an immunological checkpoint transmembrane protein, and elevated levels of expression have been linked to an unfavorable prognosis [12-14].
Transformed monocytes, T cells, and B cells are among the immune cells that express PD-1. PD-1 is an immune checkpoint receptor that is selectively targeted by Nivolumab as a monoclonal antibody. A phase 3 clinical research examining the utilization of PD-1 inhibitors uncovers the potential advantage of immune checkpoint inhibition therapy. Nevertheless, several phase 3 trials failed to demonstrate the effectiveness of PD-1 inhibition. To weigh the security and effectiveness of anti-PD-1 as an immune checkpoint inhibitor (ICI) in the management of glioblastoma, we conducted a review which were done systematically and a meta-analysis in this investigation.
Materials and methods
The PICOS (Population, Intervention, Comparison, Outcomes, and Study Design)
Individuals who are adults who have recently been diagnosed with or have a recurring case of glioblastoma (a very aggressive brain tumor classified as WHO grade IV) and have received immunotherapy with PD-1 inhibitors or standard treatment are qualified to participate in this study. Participants were required to meet the minimum age requirement of 18 years and possess a Karnofsky Performance Scale (KPS) score of at least 70. The patients were initially provided with informed consent. The intervention arm of qualifying trials consisted of Anti-PD-1 monoclonal antibodies, which act as immune checkpoint inhibitors. The control arm encompasses standard therapies for glioblastoma. Primary and secondary outcomes were examined in the studies incorporated in this analysis. The primary outcomes are median OS and PFS, while adverse events of any severity are classified as secondary outcomes. The included studies are randomized, controlled trials on glioblastoma, namely in phases I, II, and III.
Inclusion and exclusion criteria
Prior to screening, individuals who were using corticosteroids to manage symptoms of glioblastoma were instructed to discontinue or decrease their usage. This was done to ensure that the dosage of corticosteroids at the time of randomization was less than 20 mg of prednisone or less than 3 mg of dexamethasone per day. The presence of metastasis in extracranial or leptomeninges, an existing or diagnosed autoimmune disorder, concurrent consumption of a carmustine wafer and utilization of noninvasive anticancer medical device (e.g., TTF), or unresolved hemorrhage of the central nervous system were further exclusion criteria. Studies with non-human subjects, pregnant or nursing patients, the relevant data in the study but unable to be extracted, inability to communicate effectively with the neurological examiner, single-arm studies, case-series, non-randomized controlled trials (RCTs) studies, review studies, and other irrelevant articles, non-English studies were removed from the analysis.
Search methods, data collection, data appraisal, and data extraction
In adherence to the 2020 PRISMA guidelines, this study endeavored to conduct a review systematically and a meta-analysis. The Cochrane, Scopus, Pubmed, and clinicaltrials.gov databases were searched. The keyword used on each database search were "Anti-PD-1" OR "PD-1" OR "PD-L1" OR "PD-1 Inhibitor" OR "PD-1 Antibody" OR PD-1 "Monoclonal Antibody" OR "programmed death ligand-1" OR "programmed cell death-1" OR "PD-1 Transmembrane Protein" OR Nivolumab OR Ipilimumab OR Pembrolizumab AND Glioblastoma OR "Glioblastoma Multiforme" OR Astrocytoma OR "High-Grade Astrocytoma". Four authors conducted a comprehensive review of the entire text, while two authors collected the relevant information. All disputes were resolved through dialog.
Data analysis and synthesis
The results of the search were imported into Mendeley. Mendeley was utilized to exclude duplicate findings. Heterogeneity refers to the variation in study outcomes between studies and estimates the fraction of variance that is due to heterogeneity. According to the I2 value given on the forest plot using RevMan 5.4.1, heterogeneity is handled. I2 data were used to choose several effect models. The random effect model was applied when the I2 value was more than 50%. The fixed effect model was applied otherwise. The Cochrane Collaboration Tool for Assessing the Risk of Bias in Randomized Trials was utilized to evaluate the risk of bias in this investigation (RoB II). RoB II tool is a framework used to evaluate the methodological quality of randomized trials included in systematic reviews, which provides a structured approach to consider various sources of bias that can affect the results of the study.
Results
Studies selection & characteristics
In the preliminary search, 991 articles were found from four databases (361 articles from Pubmed, 435 from Scopus, 112 from Cochrane Library, and 83 from ClinicalTrials.gov). The duplicates removed were 247 articles, so the remaining 744 were screened through the titles and abstracts. Unrelated studies (n=723) were dismissed. The appropriateness of a total of twenty-one full-text publications was assessed, and subsequently, four articles were selected for inclusion in this meta-analysis, involving a total of 1677 participants. The criteria used for the exclusion were removed duplicates, non-English studies, reviews, animal studies, no report of the outcome of interest, case series, single studies, non-RCT, study protocol, and unrelated studies. Figure 1 displays the PRISMA flow diagram.
Among the studies provided, three were phase III RCTs and one was a phase I RCT. The publication year spanned from 2019 to 2022. Table 1 presents the fundamental characteristics of the RCTs incorporated in the meta-analysis. Evaluating the potential for bias in the included trials was conducted utilizing ROB2 tool (the updated Cochrane risk-of-bias methodology for RCTs). Figures 2 and 3 provide a graphical depiction of the assessment. Based on this assessment, one study was found to have a low risk of bias, which means that the researcher's execution and design reduced the bias possibility. The remaining three studies were categorized as having some concerns, suggesting that specific components of the study design or execution may have introduced bias. Some primary concerns regarding the risk of bias in all studies are the high risk of selection, performance, and detection bias.
Median OS and PFS
In our analysis, survival and disease progression rates are similar in both the group of control and the group receiving Anti-PD-1 treatment (Figures 4 and 5). From the median OS forest plot, we can summarize that the pooled hazard ratio for median overall survival was 1.08 with a p-value of 0.51. These values imply that the median OS was higher in the control group competed to the Anti-PD-1 intervention, although it was insignificant statistically. The heterogeneity addressed using I2 was 66%, so we used random analysis instead of fixed analysis for the forest plot. Moreover, subgroup analysis showed no significant differences in heterogeneity among the subgroups. In the Recurrent Glioblastoma Subgroup, the hazard ratio for Anti-PD-1 was 0.71. In Newly Diagnosed Glioblastoma, the hazard ratio for Anti-PD-1 was 1.19. These findings indicated an improved overall survival in recurrent glioblastoma subgroup. However, the confidence interval was broad.
The analysis of the median progression-free survival forest plot reveals that the pooled hazard ratio for median progression-free survival was 1.21, with a p-value=0.29. The value of hazard ratio signifies that median PFS was superior in the group of control compared to the Anti-PD-1 intervention group, although this difference did not reach the statistical significance. The I2 heterogeneity was 88%, so we used random analysis for the forest plot. Moreover, subgroup analysis shows no difference in heterogeneity among the subgroups. In the subgroup of patients with recurrency in glioblastoma, the combined hazard ratio was 0.96, indicating a slightly improved overall survival when managed with Anti-PD-1 compared to patients with new glioblastoma, who had a hazard ratio of 1.22.
PD-L1 Expression >1% and <1%
The forest plot displaying the results for PD-L1 expression levels below 1% and above 1% can be observed in Figures 6 and 7, respectively. From the Forest Plot, we can summarize that the pooled hazard ratio for survival in PD-L1 expression >1% was 1.25 with a p-value= 0.07, so it represents that survival in PD-L1 expression >1% was better in the control group than in Anti-PD-1 intervention group but not statistically significant. The heterogeneity addressed using I2 was 31%, so we used fixed analysis for the forest plot. Moreover, subgroup analysis shows no difference in heterogeneity among the subgroups. In comparison to survival in recurrent glioblastoma, survival in the newly diagnosed group exhibited a slightly higher hazard ratio of 1.25, as opposed to 1.35 in the recurrent glioblastoma subgroup. However, it still remained lower than the survival observed in the control group.
From the Forest Plot, we can summarize that the pooled hazard ratio for survival in PD-L1 expression <1% was 1.09 with a P value of 0.22, so it represent that survival in PD-L1 expression <1% was better in the control group than in Anti-PD-1 intervention group but not statistically significant. The heterogeneity addressed using I2 was 0%, so we used fixed analysis for the forest plot. Moreover, subgroup analysis shows no difference in heterogeneity among the subgroups. In contrast to the survival rate observed in newly diagnosed glioblastoma, the recurrent glioblastoma subgroup exhibited a marginally higher survival rate (hazard ratio of 0.97 vs. 1.14 in the former subgroup). Nevertheless, this survival rate remained below that of the control group. Anti-PD-1 therapy showed improved survival rates when compared to expression of PD-L1 >1%, particularly in cases where expression of PD-L1 was <1%.
MGMT promoter status
The forest plot in Figures 8 and 9 illustrates the pooled hazard ratios with respect to MGMT promoter status of methylation. Survival in the control group was superior to that of the groups undergoing Anti-PD-1 immunotherapy in both subgroup analyses of the methylated and un-methylated MGMT promoter statuses (respective hazard ratios: 1.06 for the MGMT promoter status in methylation group and 1.29 for the un-methylated MGMT promoter status group). Despite this, further research indicated that the group whose MGMT promoter was un-methylated exhibited a marginally higher survival rate than the group whose promoter was methylated. Both groups exhibited reduced survival rates in comparison to the control group. The fixed analysis revealed that the heterogeneity addressed by I2 was 0% in both forest plots.
Adverse Events
The forest plot analysis of adverse events, as illustrated in Figure 10, revealed that the control group experienced a marginally lower incidence of adverse events (1.03 risk ratio) in comparison to the Anti-PD-1 immunotherapy group while the control exhibited reduced AE, the observed disparity does not reach statistical significance (P = 0.51). However, heterogeneity addressed using I2 is 62%. Hence, random effect analysis was used for this analysis.
Discussion
Regarding PFS and OS (Figures 4 and 5), none of the incorporated studies achieved the primary endpoints for glioblastoma. All studies also showed that there are no differences in OS and PFS between Anti-PD-1 immunotherapy using Nivolumab or Pembrolizumab and the standard-of-care group [15-18]. In both OS and PFS, Anti-PD-1 showed better efficacy for recurrent glioblastoma than newly diagnosed glioblastoma. However, the differences are insignificant (p=0.51 and p=0.29 for newly diagnosed glioblastoma and recurrent glioblastoma, respectively). Despite demonstrating effectiveness in various other types of cancer, immune checkpoint inhibitor (nivolumab or pembrolizumab) does not exhibit any discernible survival advantage over the standard-of-care approach in the case of glioblastoma.
A subgroup study of newly diagnosed and recurrent glioblastoma is critical because recurrent glioblastoma frequently presents with greater severity and more treatment resistance than the initial diagnosis [19]. Significant intratumoral heterogeneity has been demonstrated in primary and recurrent glioblastomas, which may add to treatment-related complications [20]. Moreover, the genetic and epigenetic composition of the original tumor is frequently retained in recurrent glioblastoma, which may contribute in treatment resistance and the advancement of the illness [21,22]. All these elements work together to make recurrent glioblastoma more severe and difficult to cure.
Subgroup analysis of expression of PD-L1 lower than 1% and PD-L1 more than 1% yielded noteworthy results (Figures 6 and 7). To summarize, it was concluded that those with expression of PD-L1 levels below 1% had longer survival rates compared to those with PD-L1 expression levels beyond 1%. PD-L1 expression in glioblastoma has clinical relevance as it has been associated with low patient survival rate as supported by findings from other studies. High expression of PD-L1 in glioblastoma tumor tissues has been linked in a number of studies to decreased patient disease-free survival (DFS) and overall survival (OS) [23-25]. In our findings, in contrast to the group of Anti-PD-1, the standard-of-care group exhibits a higher rate of survival. Patients with recurrent glioblastoma who had PD-L1 expression levels below 1% experienced a longer period of survival compared to those with freshly diagnosed glioblastoma. In comparison to patients with recurrent glioblastoma, those with PD-L1 expression exceeding 1% exhibited a prolonged survival period among newly diagnosed glioblastoma patients. Additional research should be undertaken to ascertain these disparate findings. CD8+ T lymphocyte and interferon-gamma concentrations in the standard-of-care and Anti-PD-1 immunotherapy groups must be determined through further investigation. The reason for this is that interferon-gamma generated by CD8+ T cells induces an upregulation expression of PD-L1 [15]. Potential implications is that it has been proposed that PD-L1 expression serves as a useful therapeutic target for glioblastoma as well as a prognostic predictor [23]. The development of clinical anti-PD-L1/PD-1 treatments to elucidate the therapeutic significance of PD-L1 expression in glioblastoma are the main goals of many current researches.
MGMT, an endogenous DNA repair enzyme, contributes to preserving genomic integrity through mismatch repair [7,26]. It was known that temozolomide treatment sensitivity is directly correlated with MGMT levels [10]. However, our findings (Figures 8 and 9) highlighted the group whose MGMT promoter was un-methylated exhibited a marginally higher survival rate than the group whose promoter was methylated. Both newly diagnosed and recurrent glioblastoma groups exhibited reduced survival rates in comparison to the control group. The use of MGMT promoter status as a factor of prognosis and survival in glioblastoma is an active research area to this date [27,28]. However, the exact mechanism and it’s correlation to the tumor microenvironment of glioblastoma is developing and may be a key to a breakthrough in this field.
Although the standard-of-care group did experience treatment-related adverse events of any severity, Nivolumab's safety profile is substantial; however, these differences are insignificant statistically (p=0.51). When comparing the findings of Omuro and Reardon with those of Cloughesy and Lim, it becomes evident that the latter observed a considerably reduced incidence of treatment-related adverse events or any severity.
There are a number of research limitations: (1) further randomized studies are required to establish whether standard-of-care subgroups or anti-PD-1 immunotherapy exhibit superior survival; (2) the studies incorporated in this analysis failed to quantify the concentrations of interferon-gamma and CD8+ T lymphocytes; and (3) the studies that were incorporated failed to provide an explanation for the extended survival observed in the group of standard therapy as opposed to the Anti-PD-1 immunotherapy group. For future research suggestion, additional immuno-molecular research should be conducted to determine the reasons for the lack of substantial benefit observed with this therapy in glioblastoma, even though numerous significant Phase III randomized clinical trials have established the efficacy in using anti-PD-1 immunotherapy for various types of cancer.
Conclusion
Our findings suggest that immune checkpoint inhibitors as glioblastoma immunotherapy are not viable substitutes for standard care (surgical, radiotherapy, and temozolomide chemotherapy). In both OS and PFS, Anti-PD-1 showed better efficacy for recurrent glioblastoma than newly diagnosed glioblastoma. However, the differences are insignificant. Research on PD-L1 expression levels and MGMT promoter status might hold promising keys to immunotherapy development. Cell
therapies, alternative ICIs, vaccines, and oncolytic viruses are all additional immunotherapeutic approaches for GBM. Moreover, the investigation of ICI combined with vaccines may be undertaken.
Acknowledgments
The authors would like to express their gratitude to the Department of Immunology, Postgraduate School Universitas Airlangga, Indonesia; Lembaga Pengelola Dana Pendidikan (LPDP), The Ministry of Finance of the Republic of Indonesia; and Jalan Tengah, Indonesia (https://jalantengah.site) for editing the manuscript.
Funding
This study did not receive any funding.
Authors' Contributions
Valensa Yosephi, Peter Yustian Atmaja, Arif Nur Muhammad Ansori, and Ahmad Affan Ali Murtadlo conceived of the presented idea. Viol Dhea Kharisma, Putu Angga Wiradana, I Gede Widhiantara, Sukma Sahadewa, Maksim Rebezov, Nikolai Maksimiuk, Evgeniy Kolesnik, Marina Derkho, I Natalia Koriagina, Aswin Rafif Khairullah, Fara Disa Durry verified the analytical methods. Rahadian Zainul supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest in this study.
Orcid:
Valensa Yosephi: https://orcid.org/0000-0001-6568-080X
Peter Yustian Atmaja: https://orcid.org/0000-0001-8700-8037
Arif Nur Muhammad Ansori: https://orcid.org/0000-0002-1279-3904
Ahmad Affan Ali Murtadlo: https://orcid.org/0000-0002-7942-875X
Viol Dhea Kharisma: https://orcid.org/ 0000-0001-9060-0429
Putu Angga Wiradana: https://orcid.org/0000-0002-0139-8781
I Gede Widhiantara: https://orcid.org/0000-0003-0498-525X
Sukma Sahadewa: https://orcid.org/0009-0009-9253-7633
Maksim Rebezov: https://orcid.org/0000-0003-0857-5143
Evgeniy Kolesnik: https://orcid.org/0000-0002-2326-651X
Marina Derkho: https://orcid.org/0000-0003-3818-0556
Natalia Koriagina: https://orcid.org/0000-0001-5980-2364
Aswin Rafif Khairullah: https://orcid.org/0000-0001-9421-9342
Fara Disa Durry: https://orcid.org/0009-0003-5589-9746
Rahadian Zainul*: https://orcid.org/0000-0002-3740-3597
----------------------------------------------------------------------------
How to cite this article: Valensa Yosephi, Peter Yustian Atmaja, Arif Nur Muhammad Ansori, Ahmad Affan Ali Murtadlo, Viol Dhea Kharisma, Putu Angga Wiradana, I Gede Widhiantara, Sukma Sahadewa, Maksim Rebezov, Nikolai Maksimiuk, Evgeniy Kolesnik, Marina Derkho, I Natalia Koriagina, Aswin Rafif Khairullah, Fara Disa Durry, Rahadian Zainul*, Anti-PD-1 monoclonal antibody as immune checkpoint inhibitor for newly diagnosed and recurrent glioblastoma: a systematic review and meta-analysis of randomized controlled trials. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(5), 623-637. Link: https://jmpcr.samipubco.com/article_187678.html
----------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
