Document Type : Original Research Article
Authors
1 Department of Chemistry and Biochemistry, College of Medicine, Mustansiriyah University, Baghdad, Iraq
2 College of Medicine, University of Anbar, Ramadi, Iraq
Abstract
A chronic autoimmune condition affecting the small intestine known as celiac disease is characterized by an increase in intraepithelial lymphocytes. Despite the absence of overt malabsorption, this illness has a high frequency of bone mass derangement because of calcium malabsorption and immunological activation. This study looked at type 1 diabetes mellitus (TIDM) in Iraqis, Diabetes center in Baghdad with and without celiac disease to assess vitamin D3 and other biochemical markers. Eighty Iraqi children, aged between 4 and 16. The total number of study samples is 120 based on the number of participants in these three categories and were divided into (40) children with T1DM and Celiac disease, (20 boys and 20 girls), (40) children with T1DM without Celiac disease, (20 boys and 20 girls), and compared with (40) healthy control children, (20 boys and 20 girls). When compared to controls, there was a highly significant decrease in D3 in T1DM with celiac disease and a highly significant decrease in D3 in T1DM without celiac disease. Children with type 1 diabetes and celiac disease (CD) showed a favorable link between weight and total cholesterol (TC) and a very positive correlation between fasting blood sugar (FBS) and HbA1c in both groups (CD). We can draw the conclusion that low levels of D3 may be crucial to the onset, progression, and management of various autoimmune illnesses, including celiac disease (CD). Despite being a reasonably typical occurrence in children with diabetes, vitamin D deficiency may contribute to the disorder's early onset.
Graphical Abstract
Keywords
Main Subjects
Introduction
The loss of pancreatic beta cells in the islets of Langerhans characterizes type 1 diabetes mellitus, an autoimmune disease. Insulin insufficiency and subsequent conditions of chronic hyperglycemia are brought on by this cell death (1). Type 1 diabetes mellitus (T1DM) patients are more likely to develop other autoimmune disorders (Ads). Autoimmune thyroiditis and celiac disease (CD) are the two conditions most frequently linked (2). When gluten is consumed, celiac disease (CD), an autoimmune hereditary condition, predominantly affects the digestive system. Wheat, barley, and rye all contain the protein known as gluten. People with CD who consume gluten experience damage to the small intestine's lining, which interferes with the intestine's ability to absorb nutrients (3). Up to 1-3% of Americans are impacted by it (4). The link between type 2 diabetes and celiac disease was originally discovered in the 1960s. Moreover, the average prevalence of diabetes and celiac disease was 4.5%. (5). Similar triggering of autoimmune processes has been reported in type 1 diabetes and celiac disease, which share a hereditary basis linked to HLA DQ2 or HLA DQ8 (6). IgA and IgG anti-gliadin antibodies are created in reaction to gliadin (wheat prolamin). Three distinct alleles that each encodes gliadin can result in the production of a different type of antibody. Eighty percent of celiac disease patients have anti-gliadin IgA antibodies (7). These antibodies work to stop killer cells from destroying intestinal villus epithelial cells in celiac disease by destroying the villus extracellular matrix (8). Globally, vitamin D insufficiency is common (9). Several epidemiological studies have discovered that type 1 diabetic children and adolescents have a high frequency of vitamin D insufficiency (VDD) (10) proof that low vitamin D levels or vitamin D deficiency may be risk factors for type 2 diabetes and type 1 diabetes (T2D) and increased glycated hemoglobin concentrations (11). Children and adolescents with T1D frequently have VDD (12,13). In this study, type 1 diabetes in Iraqi children of type 1 diabetics with and without celiac disease was assessed using vitamin D3 and other biochemical markers.
Materials and methods
Eighty Iraqi children, aged between 4 and 16, who were enrolled in the Diabetes center in Baghdad from October 2022 to December 2022. The total number of study samples is 120 based on the number of participants in these three categories that are divided into (40) children with T1DM and Celiac disease (20 boys and 20 girls), (40) children with T1DM without Celiac disease (20 boys and 20 girls), and (40) healthy control children (20 boys and 20 girls). All patients' information, including their sex, age, weight, height, and body mass index, was gathered (BMI). Using automated Cobas instrumental methods, serum fasting blood sugar (S.FBS), lipid profile (serum total cholesterol (S.TC), serum triglyceride (S.TG), and serum high density lipoprotein (S.HDL-C), blood urea (B. urea), and serum creatinine (S. creatinine) were estimated (14). The Student-t test was used to assess whether a difference in mean values between two groups was significant (a P-value of less than 0.05 was considered significant).
Results
Table 1 indicates that there are significant differences among groups of patients in T1DM with CD (G1), T1DM without CD (G2) and healthy (G3) subjects. The statistics view that there is no significant in groups for each of the age and high. A highly significant different increase at (P <0.001) was recorded between G1 vs. G3, G1 vs. G2 and G2 vs. G3 for each of FBS, HbA1c, TC, and LDL-C, while a significantly different increase (P <0.05) for TG. Also, a highly significant difference decreased (P <0.01) for vitamin D3 among three groups while significant difference decreased (P <0.05) for HDL-C among three groups.
Table 2 presents a substantial positive association between weight and TC in both groups of children with type 1 diabetes and celiac disease (CD), as well as a highly positive correlation coefficient between FBS and HbA1c in both groups (CD). While there is no association between age, high TG, and HDL-C in either group of children with type 1 diabetes and celiac disease (CD).
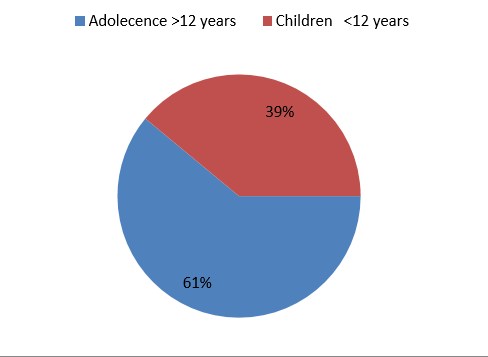
Figure 1 shows that children (39%) had higher rates of vitamin D3 deficiency in T1DM with celiac disease than adolescents (61%). The vitamin D3 deficiency in children (39%) compared to adolescents (61%) in T1DM without celiac disease is also shown in Figure 2.
Discussion
The information provided here demonstrates that the vitamin D3 levels of the study subjects (including those with and without T1DM) were less than 30 ng/ml. These results are consistent with those of other research of a similar nature, including Ginde AA. et al. (2009) (15). Also, there was a significant link between the levels of vitamin D3 in T1DM patients with CD and T1DM patients without CD (8.62±1.00, 9.38±2.37 mg/dl with control (33.33±5.91 mg/dl), P-value (0.0001), in CD patients. According to Krupa-Kozak et al. (2014), VD deficit resulting from malabsorption may be the primary factor causing various clinical signs of the disease, including decreased bone mineral density, decreased bone mass, and increased bone fragility (16). It is fair to assume that VD may also affect CD given the well-documented effects of VD on the immune system and gastrointestinal tract in vitro and in vivo. Vitamin D (VD) may have a role in regulating the onset and course of CD, according to the evidence that VD can shield intestinal mucosa from chemical and immunological harm and that VD can counteract immune system actions that result in the intestinal modifications typical of gastrointestinal autoimmune diseases (17,18). Infantino et al. (2022) (19). Individuals born in the summer are more likely to have a VD deficiency than those born in the winter, when autoimmunity may develop and people may first experience gluten exposure (20). Recent research has demonstrated that VD may perform a variety of extra-skeletal tasks, primarily through modulating the innate and adaptive immune systems in an appropriate manner (21). As a result, it has been hypothesized that VD may be crucial to the genesis, clinical course, and management of a number of autoimmune illnesses, including celiac disease (CD) (22). The discovery that chronic dietary gluten exposure in genetically predisposed subjects always results in the production of autoantibodies against transglutaminase 2 (TG2), an enzyme that is essential for gluten-induced pathogenesis in CD (23), provides the strongest evidence yet for the autoimmune origin of this disease. The VD3 levels between adolescents and young children in T1DM with Celiac Disease (Figure 1) revealed that the percentage of adolescents with CD was higher than that of patients without CD, which is in accordance with Unalp-Arida, A. et al. (2017) (24). This hypothesis has been strongly supported by the evidence, which shows that in some circumstances, such as those with potential VD hypovitaminosis, the risk of CD development is higher. Several studies have also shown that CD is more prevalent among residents of northern regions, where exposure to sunlight or UVB radiation is lower and skin synthesis of VD is also lower, particularly for children, for whom an appropriate VD intake is required for bone growth and development (19). There is a significant correlation between the VD levels in CD and control children (8.62±1.00) and (33.33±5.91), respectively, (P=0.0001), which is in agreement with Lionetti, E. et al. (2021) (25). Various cofactors, including the month of blood testing, the patients' racial makeup, and the sort of diet they were given, may have an impact on VD concentrations and cause the discrepancies in the results.
Gluten peptides attach to human leucocyte antigens on antigen-presenting cells as they pass through the permeable intestinal mucosa and are deamidated by tissue transglutaminase, changing adaptive immunity in CD patients. The inflammatory response causes the recognizable mucosal ulcers when Th1 cytokines are released, activating T-cells and CD4+ (26).
The findings given here demonstrate that our patients' HbA1c values with control (12.79±4.74), (9.92±2.35), and vas control (5.20±0.46) exhibited positive significant correlations, respectively (0.001). According to Tuba Bulut et al. (2017)'s study, levels of triglycerides, LDL cholesterol, and total cholesterol were significantly higher than the control, it may the result of insulin resistance were occur in obese subjects (27).
Conclusion
The development, clinical course, and management of various autoimmune illnesses, including celiac disease (CD), may be significantly influenced by low levels of vitamin D3. Although vitamin D deficiency is a relatively common occurrence in children with diabetes, it may be a possible cause of the early development of the disorder, our suggestion to give them vitamin D as a supplementation to decrease the disorder.
Acknowledgements
The research presented here was accomplished with assistance from " Diabetes Center in Baghdad". We would want to express our appreciation to each and every person who took part in this research.
Funding
The money was cashed on this research from the authors( Dr.Sahar and Dr .Methal).
Conflict of Interest
The authors declared no conflict of interest.
Orcid:
Sahar Abdul Wahab ALShaban*: https://orcid.org/0000-0001-8330-7160
Mithal R. Alkubaisi: https://orcid.org/0000-0003-3283-1186
---------------------------------------------------------------------------------------
How to cite this article: Sahar Abdul Wahab ALShaban*, Mithal R. Alkubaisi, Evaluation of vitamin D3 levels in iraqi type I diabetes mellitus with and without celiac disease. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(6), 675-681. Link: https://jmpcr.samipubco.com/article_187947.html
---------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
