Document Type : Original Research Article
Authors
- Tirandan Menoer Elliza Primalia 1
- Damayanti Tinduh 1
- I Putu Alit Pawana 1
- Sony Wibisono Mudjanarko 2
- Budi Utomo 3
1 Department of Physical Medicine and Rehabilitation, Dr. Soetomo General Academic Hospital, Faculty of Medicine, Airlangga University, Indonesia
2 Department of Internal Medicine, Dr. Soetomo General Academic Hospital, Faculty of Medicine, Airlangga University, Indonesia
3 Department of Public Health and Preventive Medicine, Faculty of Medicine, Airlangga University, Indonesia
Abstract
Diabetes mellitus (DM) patients can have complications of neuropathy and angiopathy in the feet. Both of these conditions increase the risk of diabetic foot ulcers and the risk of falls. Screening for ulcer risk as early as possible is important for type 2 DM patients, as is assessing the risk of falls. Ulcer risk assessment using the International Working Group of Diabetic Foot (IWGDF) criteria shows high sensitivity, as does the Timed Up and Go (TUG) test in assessing fall risk. Studies on the risk of falls in adult DM patients associated with the risk of ulcers are still limited in Indonesia. The study subjects comprised 48 type 2 DM patients aged 18-59 years without active foot ulcers and a history of amputation. All subjects underwent an assessment of the level of ulcer risk stratification based on IWGDF criteria and TUG testing in one visit. Correlations between variables were assessed in an analytical observational study with a cross-sectional design. The analysis showed a significant relationship between the risk level of foot ulcers and the TUG value (p=0.03). The TUG values at all risk levels have a significant comparison (p = 0.003). Significant differences were found between very low and low risk, very low and moderate risk, and moderate and high-risk groups. The risk level for foot ulcers was also significantly related to HbA1C levels (p = 0.005). There was a significant relationship between the level of ulcer risk stratification and the risk of falls in patients with type 2 diabetes mellitus at Dr. Soetomo Surabaya General Hospital.
Graphical Abstract
Keywords
- Foot ulcer risk
- IWGDF risk stratification
- diabetic foot
- diabetic foot ulcer
- risk of falls
- timed up and go
Main Subjects
Introduction
The World Health Organization (WHO) states that there has been an exponential increase in cases of all types of diabetes mellitus (DM) in recent decades throughout the world. The prevalence of DM increased from 108 million (4.7%) in 1980 to 425 million (8.5%) in 2017 and is expected to be 629 million in 2045. Southeast Asia accounted for 82 million DM cases, which is 19.3% of the total world DM cases after the West Pacific had 159 million cases, which is 37.4% of the world's total DM cases [1]. The prevalence of DM reported by the Data and Information Center of the Ministry of Health from the results of Basic Health Research (Riskesdas) in 2013 stated that the proportion of diabetes mellitus in the population aged over 15 years was recorded at 6.9% and there was an increase to 8.5% in 2018. Group aged 35-44 years has a prevalence of 1.1%, age 45-54 years is 3.9%, and age 54-64 years is 6.3% in Indonesia [2].
One of the complications of diabetes mellitus is diabetic feet, both with and without ulcers. The lifetime incidence of foot complications in DM patients is estimated to be between 15% and 25%. The global prevalence of diabetic foot ulcers is 6.3%, with more Type 2 DM patients than Type 1 DM patients [3]. Cases of Type 2 DM (T2DM) treated at RSUD Dr. Soetomo Surabaya's association with foot ulcers was 9.08%, where the rates of lower extremity amputation and death were 14.11% and 40.93%, respectively [4]. The mortality rate in patients with diabetic foot ulcers is 2.5 times higher than in DM patients without ulcers [5].
Diabetic foot is a significant contributor to the global burden of disability and reduced quality of life. Diabetic foot imposes a substantial economic burden on the health care system, including direct and indirect costs and loss of personal income [6]. The cost of diabetic foot ulcers without lower limb amputation ranges from US$993 to US$17,519 and increases to US$43,800 for minor lower limb amputation and US$66,215 for major lower limb amputation. Most expenses are not just for surgery but include rehabilitation medicine, nursing homes, and internal medicine. Prevention of diabetic foot ulcers and lower extremity amputations may be the most effective way to reduce high treatment costs [7].
Diabetes mellitus also plays a role in the risk of falls. Diabetes mellitus can affect the sensory organs in the feet, resulting in an increased risk of falls, fractures, and death [8]. The risk of falls was higher in DM patients [9,10]. Falls are also common in individuals with DM and a history of foot ulcers [11]. Patients with diabetic foot ulcers are twice as likely to fall and have a threefold higher risk of fracture than patients without ulcers. Sixty-three percent of patients with a history of diabetic foot ulcers experienced a fall during the two-year follow-up period. Diabetic neuropathy is considered the most dominant mediator between diabetes and falls. DM patients with diabetic neuropathy have a 20 times greater risk of falling than healthy people [12,13]. Subjects with PAD also had a 73% greater history of falls than healthy subjects. Nerve dysfunction in the lower extremities of PAD subjects due to impaired peripheral circulation is a potential mechanism for increasing the prevalence of falls [14].
Falls are one of the most common injury mechanisms and have been a major cause of morbidity and mortality globally in the last three decades. The main causes of disability in fall victims are fractures of the patella, tibia or fibula, and ankle. Falls can result in a patient suffering disability, loss of income, dependency on caregivers, and environmental accessibility preferences. The highest mortality-to-incidence ratios (MIR) values are found in Southeast Asian countries such as Indonesia, Cambodia, Myanmar, and Vietnam, exceeding 0.03. This value indicates an average of more than three deaths per 100 falls [15]. Falls result in more years lived with disability than transport injuries, drowning, burns, and poisoning combined [8]. Fall-related injuries are expected to double by 2030 due to the increased risk of falls. Assessing fall risk in young to middle-aged diabetes patients is warranted for early identification and appropriate rehabilitation [16].
Diabetic foot is a multifactorial condition, so understanding the clinical factors that influence morbidity will increase the success of prevention and treatment. Risk stratification of diabetic foot ulcers based on assessment by the IWGDF demonstrated high accuracy in a prospective external multicenter validation study with a sensitivity of 98% and a specificity of 58%. The IWGDF guidelines were updated in 2019 based on a systematic literature review and formulation of recommendations by multidisciplinary experts worldwide [17,18].
Screening for ulcer risk as early as possible is important for type 2 DM patients, as is assessing the risk of falls. Studies on the risk of falls in adult DM patients associated with the risk of ulcers are still limited. Researchers consider it necessary to examine the relationship between the risk of ulcers and the risk of falls in type 2 DM patients at Dr. Soetomo Surabaya Hospital.
Experimental
Methods
This research is an analytical observational study with a cross-sectional design at the Medical Rehabilitation Installation of Dr. Soetomo Surabaya Hospital. This research received a certificate of ethical suitability from the Health Research Ethics Committee of Dr. Soetomo General Hospital Surabaya with no. 0603/KEPK/II/2023.
Inclusion criteria: 1) Type 2 DM patients; 2) Age 18-59 years; 3) Stable hemodynamics; 4) Normal cognitive function; 5) Able to walk independently without walking aids or lower limb prosthesis; and 6) Willing to participate in this research voluntarily by signing a consent form to become a research subject (informed consent).
Exclusion criteria: 1) Active ulcers or signs of acute inflammation in the lower limbs; 2) There was a history of amputation of the lower limbs; 3) Hypoglycemia conditions (GDA <70mg/dL); 4) Hyperglycemia conditions (GDA³250mmHg); 5) Cardiorespiratory complaints that affect physical performance (such as NYHA class 3-4 heart failure, acute heart attack, unstable angina, uncontrolled arrhythmia, aneurysm, severe aortic stenosis, acute endocarditis/pericarditis, persistent asthma, and acute respiratory failure or heavy); 6) Neuromusculoskeletal diseases that interfere with ambulation function; and 7) Uncorrected visual impairment. Criteria for dropping out: The subject states that he has withdrawn or died.
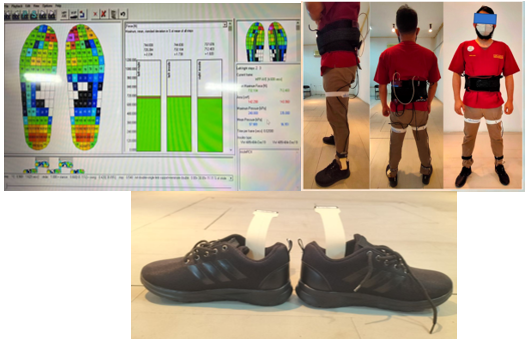
Research instrument
This study used a digital sphygmomanometer, stethoscope, pulse oximeter, thermometer, body scales, and height-measuring instrument to obtain basic patient data. The stick method blood sugar measurement tool assessed subjects' random blood sugar before data collection. A 10G monofilament (5.07 Semmes-Weinstein) and a vascular Doppler device were used to determine LOPS and PAD so that subjects could be classified according to the level of ulcer risk. In-shoe pressure measurement in the form of a Pedar-X device and a metronome is used to assess plantar pressure. A standard chair and stopwatch are also required in the timed up-and-go test.
Basic data and examination results are recorded on the data collection sheet. Emergencies and falls are anticipated by providing a cold pack and emergency kit consisting of one unit of an oxygen cylinder, mask and oxygen hose, Ambu bag, 2 mL epinephrine injection, 3 mL injection syringe size 23G, 1 mL injection syringe size 23G, povidone-iodine, sterile gauze, and plaster.
Data were analyzed computerized with SPSS v20.0 using the Spearman Test to compare the risk of foot ulcers and falls in type 2 DM sufferers.
Results
This study obtained 48 subjects who met the inclusion and exclusion criteria. There are more female subjects than male subjects, with a body mass index of 26.5 4.33 kg/m2. The average age of the research subjects was 49.81-7.21 years, with the data normality test result being p = 0.01, where the age data was not normally distributed. Most of the study subjects received insulin therapy. The research subjects had an average duration of suffering from T2DM of 6.78 years and an HbA1c level of 8.20%. All subjects had one or several comorbidities, including hypertension, heart disease, and dyslipidemia. Foot pressure in peak pressure was also checked for all subjects, with an average value for the right foot of 223.73±55,22 kPa and 214.37±38.5 kPa. Subjects classified as very low risk had the largest number, followed by subjects with low, medium, and high risk (Table 1). Subject characteristics, along with TUG values for each level of ulcer risk stratification, are presented in Table 2.
Foot ulcer risk stratification was significantly associated with TUG value (p = 0.03) (Table 3). There was no significant relationship between T2DM duration, body mass index, and foot ulcer risk classification (p = 0.6). There was also no relationship between HbA1c levels, DM duration, and body mass index with TUG values (p > 0.05).
Diagram of the relationship between foot ulcer risk stratification and TUG value in Figure 1 and Diagram of the relationship between foot ulcer risk stratification and HbA1C levels in Figure 2. The correlation test of subject characteristic variables with TUG is indicated in Table 4. A comparison test of TUG values between foot ulcer risk stratification levels is provided in Table 5. Comparison test of TUG values at each level of foot ulcer risk stratification in Table 6.
The TUG value at all risk stratification levels was significantly compared with the values = 0.003 based on the ANOVA test. The LSD test illustrates that there is a significant comparison between very low-risk stratification and low risk with a value of p = 0.006 and between very low and high-risk stratification with a value of p = 0.03. The TUG value between medium and high-risk stratification also has a significant difference with a p-value = 0.12.
Discussion
This study is an analytical observation study that uses one assessment group. This is intended to provide information regarding the pressure on the soles of the feet of people with type 2 DM and its relationship to the level of stratification of foot ulcers. Researchers have tried to minimize the risk of bias by applying inclusion and exclusion criteria. The distribution of data on age, body mass index, duration of suffering from type 2 DM, and HbA1c levels was obtained with p-values> 0.05, so they were normally distributed.
The study subject recruitment process resulted in 48 subjects. Table 5 indicates that most research subjects were women (54.2%) and men (45.8%). This is the same as the prevalence of T2DM in Indonesia, which is predominantly suffered by women [2]. The risk of foot ulcers in T2DM patients is assessed by several factors: foot sensory function, peripheral arterial disease, foot deformity, and a history of end-stage renal disease. These conditions cannot be separated from the influence of the duration of a person suffering from T2DM, HbA1C levels, treatment received, and other comorbidities that worsen hyperglycemia conditions, such as a body mass index status that is more than normal [19,20].
The average HbA1C level in research subjects was 8.20. This shows that most subjects have uncontrolled blood sugar levels, where the expected target HbA1C in T2DM sufferers is less than 7% [21]. The average duration of T2DM obtained from all subjects was 6.78 years, where the longer a patient has diabetes, the greater the risk of DM complications that can occur [22,23]. The mean body mass index of the research subjects was 26.5 kg/m2, classified as obese. This can reduce insulin sensitivity and worsen hyperglycemia conditions so that the risk of foot ulcers increases [24].
Data analysis shows a p-value = 0.03 in the relationship between the level of risk stratification and the TUG value. This shows that the increase in the risk of foot ulcers is proportionally and significantly related to the TUG value, where the higher the risk of eating ulcers, the higher the TUG value, so the greater the risk of falls. This supports previous research where an increased risk of ulcers will affect the dynamic balance and risk of falls in T2DM patients. Diabetes mellitus is associated with slower gait speed, lower lower extremity function, decreased balance, and increased risk of falls in female subjects [25]. Instability related to diabetic neuropathy is common. A large-scale study in the UK and USA showed that 23% of 484 patients with diabetic neuropathy considered themselves unstable due to balance problems [13]. A similar study in Pakistan also found that 92% of T2DM patients had neuropathy, and 75.5% of patients were labeled as delayed for TUG results [26].
Patients with DM experience changes in walking strategy, decreased walking speed, reduced range of motion, and joint moments. Young to middle-aged South African adult subjects with diabetes had a higher risk of falls when compared with those without diabetes [13,16]. Patients with polyneuropathy walk more slowly than DM patients without neuropathy. DM and polyneuropathy patients also adopt a wider stride to increase stability and provide a greater base of support when standing. Still, the process of walking involves a constant transition between the legs, requiring balance on one leg while advancing the other leg forward. The center of mass of the body needs to move towards the side of the foot in the stance phase when walking so that a wider step can cause greater displacement between sides, cause balance disorders, and increase instability in patients with DM and diabetic polyneuropathy [13].
Long-term hyperglycemia can cause progressive damage to sensory nerve fibers. Diabetic neuropathy is considered the most dominant mediator between diabetes. It falls because decreased lower extremity somatosensation reduces the ability to detect changes in balance and make appropriate adjustments to avoid falls [12]. Loss of sensory function in the feet causes changes in gait biomechanics, affects balance, and is a major risk factor for falls [13].
The significant correlation between the level of risk stratification and the TUG value is also similar to previous studies, where it was found that patients with PAD experienced prolonged TUG values. Patients with PAD experience difficulty walking, possibly due to effort intolerance arising from poor foot perfusion and impaired functional mobility of the lower extremities during walking [27]. A linear analysis showed increased variability in gait patterns in PAD patients. Symptomatic PAD patients experience increased gait variability in the ankle, knee, and hip joints at the start of ambulation, even without claudication pain. These findings suggest a significant impairment in the function of the locomotor system of symptomatic PAD patients. This results in gait instability and is a potential contributing factor to the falls and mobility problems experienced by symptomatic PAD patients [28].
This study found increased TUG values in subjects with a history of foot ulcers. This is similar to previous research where, after 1 year, 54% of subjects reported at least one fall. The overall incidence of falls in the study was 1.25 falls/person per year. 41% of subjects even reported falling twice or more. Patients with a previous history of diabetic foot ulcers who have one or more comorbidities and foot numbness were identified as the main risk factors underlying falls [11,13].
The relationship between the level of risk stratification and HbA1C levels has a value of p = 0.005. This shows that the risk of foot ulcers is proportionally and significantly related to HbA1C levels. Research in 2016 had similar results, finding that subjects who had poor blood glucose control were 5.8 times more likely to experience ulceration than those who had good blood glucose control [29]. 63% of 1524 T2DM study subjects experienced complications related to glycemic control with HbA1c values > 7.5 g/dl [30]. Differences in HbA1c levels, according to Nyamu, Otieno, Amayo, and Mcligeyo in 2003, showed an average HbA1c of 9.63%, which could cause foot ulcers. The results of another study found that subjects with an average HbA1c value of 8% with a standard deviation of 1.4 suffered from foot ulcers [31].
A study in Japan found that normalizing HbA1c in type 2 diabetes with a short period could improve microvascular complications, including neuropathy, more effectively [30]. Subjects with higher HbA1c levels showed lower amplitudes and reduced motor nerve conduction velocities in the tested nerves. Lower sensory nerve conduction velocities were also observed in the sural nerve. HbA1c variability with chronic glycemic disorders is strongly associated with the severity of peripheral neuropathy in patients with type 2 diabetes.
Increased levels of advanced glycation end products (AGE) and protein kinase C (PKC) due to prolonged hyperglycemia are thought to be involved in peripheral nerve damage. Oxidative stress caused by AGEs creates microscopic blood vessel damage, inhibiting blood supply to peripheral nerves. Certain proinflammatory cytokines, including IL-6 and TNF-α, are also increased during hyperglycemia and are thought to contribute to nerve cell damage [32].
Intensive glycemic control and lower HbA1c levels are accompanied by a decrease in diabetes complications where HbA1c <7% is associated with a 60% reduction in the incidence of peripheral neuropathy. Research shows that high HbA1c levels can cause peripheral diabetic neuropathy. Patients with high HbA1c levels should be considered at risk for diabetic foot complications and receive preventative education from a podiatrist [33].
Another method that can be used to monitor glycemic control is the use of continuous glucose monitoring systems (CGMS). This system provides glucose measurements throughout the day to determine fasting and postprandial blood glucose levels for better insulin dose adjustment, the effect of exercise or physical activity on glucose levels, and the detection of undetected hypoglycemia or hyperglycemia. Monitoring glucose variability is also as important as measuring HbA1c, fasting plasma glucose, and postprandial glucose because fluctuations in glucose levels are powerful activators of oxidative stress. Continuous glucose monitoring systems allow index detection of mean amplitude glucose excursions (MAGE), which is the gold standard for determining glucose variability. This allows the prevention of hypoglycemic episodes and allows diabetics to maintain physiological glucose concentration levels, i.e., euglycemia with reduced glycemic variability [34].
The advantages of CGMS in diabetes management are clear as diabetics can continuously monitor their glucose levels, which have been shown to significantly reduce HbA1c levels and maintain them for long periods of time without changing the daily insulin dose. Because it previously showed long-term benefits for reducing HbA1c levels. The use of CGMS, previously limited to individuals with type 1 diabetes mellitus, is now rapidly increasing in the T2DM population. All current CGMS devices are accurate enough for safe and effective diabetes management. The glycemic benefits of all devices have also been proven in various clinical trials [34,35].
This study produced a p-value = 0.6 for the correlation between the level of risk stratification and the duration of T2DM. These data suggest that the risk of foot ulcers is not related to the length of time a person suffers from T2DM. This is in contrast to some studies where patients in the high-risk group had a longer duration of diabetes [20,36].
This condition is possible because the risk of foot ulcers is also influenced by hyperglycemia. Some subjects had controlled HbA1C levels even though they had suffered from T2DM for longer than others with uncontrolled HbA1C values. Previous research had all subjects with uncontrolled blood glucose levels in addition to a longer duration of diabetes (> 10 years), so a significant relationship was found between the duration of T2DM and the risk of ulcers [20,36].
A similar thing was also found in the relationship between BMI and the level of ulcer risk stratification, resulting in a p-value = 0.6. This condition is in line with the study conducted by Huang et al., where no relationship was found between BMI and the recurrence of leg ulcers. Diabetic neuropathy and peripheral arterial disease are more closely related to the risk of diabetic foot ulcers [37].
This study had subjects with mean peak pressure values of 223.73±55,22 kPa and 214.37±38.5 kPa, which did not have a significant relationship to the risk of foot ulcers with p values of 0.7 and 0.8, respectively. An Egyptian study suggested a cut point of 355 kPa for peak pressure to indicate a high risk of ulceration, which would be more valid when used in conjunction with other contributing risk factors, namely, duration of diabetes, smoking, glycemic load, foot deformity, and severity.
Research by Chatwin and colleagues suggests that assessing cumulative pressure applied over time may be a more relevant parameter than peak pressure. This is based on previous studies that focus on peak pressure when walking while a person's activities are considered to be longer spent on other activities where lower foot pressure is applied for a longer duration [39]. Other studies suggest that the location of the measurement area should be considered when assessing the relationship between peak pressure and sole ulceration [40].
Apart from plantar pressure, the risk of foot ulcers in diabetes patients is also influenced by metabolic syndrome, including dyslipidemia, which is found in 89.61% of T2DM patients [41,42]. This study also did not control the subjects' physical activity or exercise, so it could have an effect on glycemic control. Moderate-intensity physical exercise can increase the number of pancreatic β cells and the average area of the islets of Langerhans [43]. Moderate-intensity treadmill exercise with gradual increases in speed and incline was found to provide better results in increasing adiponectin levels than standard individual physical exercise in managing T2DM [44]. Adiponectin can inhibit the production of proinflammatory cytokines, increase the production of vascular endothelial growth factor, a key mediator of angiogenesis, and inhibit the activation of the intrinsic apoptotic pathway. In addition, adiponectin is known to have antioxidant properties and impacts glucose metabolism, the immune system, extracellular matrix remodeling, and nerve function. Available evidence suggests that adiponectin and its receptor agonists may be useful as therapeutic targets for the management of DFU [45]. Moderate-intensity treadmill exercise with a gradual increase in incline for 30 minutes three times/week for four weeks has also been shown to improve balance function [46]. Another systematic review shows that there are local microclimate factors that are also involved in the development of foot ulcers, including temperature, humidity, and the coefficient of friction of the soles of the feet [47].
This study did not find a significant relationship between HbA1c, duration of DM, body mass index, and peak pressure on TUG. The risk of falls in T2DM patients is influenced by age, gender, duration, and treatment of DM, diabetic neuropathy, diabetic retinopathy, vestibular disorders, muscle weakness, limited joint movement, and degenerative changes that occur in the brain [13,48]. Diabetic neuropathy is considered to be the most dominant mediator between diabetes and falls [12]. Diabetic neuropathy is more related to glycemic control (HbA1C) than the age and duration of someone suffering from DM [20]. The severity of the diabetic neuropathy condition, which could affect the patient's balance in this study, was not measured quantitatively. A similar thing was also found between BMI and TUG, where glycemic control and the severity of diabetic neuropathy played a role in the risk of falls in DM patients [13].
The TUG value at all levels of risk stratification has a significant comparison with a p-value of 0.003. Significant differences were mainly found between very low and low risk, very low and moderate risk, and moderate and high-risk groups. The very low-risk group is subjects with T2DM who do not have symptoms in the legs. The low, medium, and high-risk groups are subjects with symptoms such as loss of protective sensation/decreased sense of touch, foot deformities, peripheral arterial disease, and a history of foot ulcers [18].
Symptoms obtained at each level of foot ulcer risk stratification can cause changes in gait patterns that affect the dynamic balance of patients with diabetic feet. The prolonged hyperglycemia that occurs in T2DM stimulates a series of metabolic interactions that cause endoneural hypoxia and alter nerve perfusion, including peripheral nerves. Diabetic neuropathy can alter movement perception as a result of reduced proprioceptive and cutaneous input from the skin, muscles, and joints [48]. Patients with diabetic polyneuropathy also show decreased muscle mass, intrinsic muscle strength of the foot and ankle, and decreased intra- and intermuscular fat accumulation. This can then cause foot morphological abnormalities [13].
Another study found that variations in foot morphology increased the risk of falls in elderly adult subjects. Subjects with hallux abductus valgus and bunions had twice the risk of falls than the control group [49]. The incidence of peripheral neuropathy, slower gait speed (p<0.001), increased vibration threshold (p=0.04), and decreased muscle strength for dorsiflexion, plantarflexion, inversion, and eversion (p<0.001) were found in the group with foot deformity [50]. Ankle flexibility, sole tactile sensitivity, and finger plantar flexor strength were also significant and independent predictors in balance and functional tests of elderly subjects [51].
This study obtained lower TUG values in the moderate ulcer risk group than in the low ulcer risk group. This is possible because all moderate-risk subjects in this study were subjects with an ABI value <0.9, which indicates PAD, without using subjects with leg deformity. Diabetics with foot deformities that cause deviations in gait patterns and those who were unable to step on all parts of the sole of the foot were excluded from this study in order to obtain a gait pattern that was as uniform as possible for all subjects. However, foot deformity, on the other hand, is considered predictive and strongly associated with foot ulceration [52]. Previous laboratory research also stated that the thickness of the cortical bone in diabetic mice was 18% lower than in normal mice [53]. Bone thickness is further related to the incidence of deformity [54]. All subjects also did not undergo diagnostic examinations related to the arch of the foot. Several methods can be used to assess the arch of the foot, one of which is using the Staheli Index, which has been researched to have the best performance for diagnosing flatfoot in athletes [55].
Subjects with peripheral arterial disease also had a 73% greater history of falls than healthy subjects. Nerve dysfunction in the lower extremities of PAD subjects due to impaired peripheral circulation is a potential mechanism for increasing the prevalence of falls [14]. Patients with diabetic foot ulcers are at greater risk of falls. Sixty-three percent of patients with a history of diabetic foot ulcers experienced a fall during the two-year follow-up period [13].
This study had a population of T2DM patients without a control group, so there was no comparison in the form of TUG values in healthy subjects. The subjects included in this study did not include elderly subjects, with the sample size for each level of ulcer stratification being uneven. This research also did not use other balance-checking instruments or quantitative gait analysis. Studies regarding the correlation between the level of stratification of foot ulcers and balance function still require further study based on these conditions. Recommendations for future research could consider sample size for each level of ulcer stratification, age range, use of other balance assessment instruments, and quantitative gait analysis.
Bias factors that are still difficult for researchers to control are physical activity, daily intake, medication compliance, and vascular disease other than peripheral arterial disease. These four factors can influence the subject's hyperglycemia and vascular conditions, which have an impact on the risk of foot ulcers. Foot care and the thickness of the foot fat pad will also affect the condition of the subject's feet and walking patterns, which will have an impact on balance function.
Conclusion
There is a correlation between the level of ulcer risk stratification and the risk of falls in patients with type 2 diabetes mellitus. Patients who have a higher risk of ulcers show a higher risk of falls.
Supporting Information
Not applicable.
Acknowledgements
All staff at Physical Medicine and Rehabilitation, Dr. Soetomo General Academic Hospital, Faculty of Medicine, Airlangga University, Indonesia, all author and all patient.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' Contributions
Conceptualization, data analysis, and drafting: Tirandan Menoer Elliza Primalia. Review and revising: Damayanti Tinduh, I Putu Alit Pawana, Sony Wibisono, Budi Utomo
Conflict of Interest
No potential conflict of interest relevant to this article was reported by the authors.
Orcid:
Tirandan Menoer Elliza Primalia*: https://orcid.org/0009-0002-8871-3365
Damayanti Tinduh: https://orcid.org/0000-0001-6604-8152
I Putu Alit Pawana: https://orcid.org/0000-0002-6775-964X
Sony Wibisono Mudjanarko: https://orcid.org/0000-0002-2339-5266
Budi Utomo: https://orcid.org/0000-0001-6060-9190
-------------------------------------------------------------------------------------------
How to cite this article: Tirandan Menoer Elliza Primalia*, Damayanti Tinduh, I Putu Alit Pawana, Sony Wibisono mudjanarko, Budi Utomo, Correlation between the level of foot ulcer risk stratification and the risk of fall in type 2 diabetes mellitus patients at dr. soetomo surabaya general hospital. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(6), 701-715. Link: https://jmpcr.samipubco.com/article_188333.html
-------------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
|
|

.png)
.png)
.png)
.png)
.png)
.png)
