Document Type : Case Report
Authors
1 Department of Ophthalmology, Dr. Soetomo General Academic Hospital, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
2 Department of Dermatovenereology, Dr. Soetomo General Academic Hospital, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
Abstract
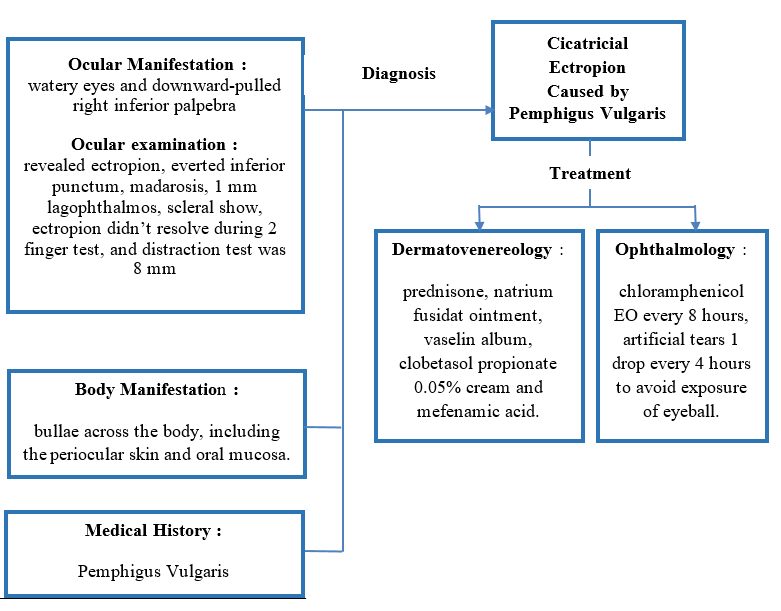
Pemphigus vulgaris is a rare autoimmune disorder that arises from autoantibodies targeting antigens in intraepidermal cell cohesion, leading to painful erosions and flaccid blisters. Given that pemphigus vulgaris can induce cicatricial ectropion, a comprehensive diagnosis and treatment is essential. A 61-year-old man was referred from a dermatovenereology clinic with a two-month history of watery eyes and a downward-pulled right inferior palpebra. The initial manifestation involved bullae across the body, including the periocular skin and oral mucosa. The visual acuity (VA) in his right eye was 5/6, and in his left eye, it was 5/12. The examination of his right eye revealed ectropion, an everted inferior punctum, madarosis, 1 mm lagophthalmos, scleral show, and ectropion that did not resolve during the 2-finger test, with a lid distraction of 8 mm based on the distraction test. Despite blinking during the snap-back test, his inferior palpebra did not return to its normal position. The diagnosis of cicatricial ectropion caused by pemphigus vulgaris was made. Cicatricial ectropion is the outward rotation of the eyelid margin due to anterior lamella shortening from scar tissue. This shortening leads to the eyelid margin moving away from the eyeball, causing watery eyes, irritation, and cosmetic concerns. Lubrication treatment for the patient's eyes included chloramphenicol eye ointment every eight hours and artificial tears (1 drop every 4 hours) to avoid exposure of the eyeball. The treatment administered in the dermatovenereology clinic consisted of prednisone, natrium fusidate ointment, vaselin album, clobetasol propionate 0.05% cream, and mefenamic acid. Scar tissue in the anterior lamella caused by chronic inflammation of periorbital pemphigus vulgaris could result in ectropion. The management aimed to protect the eyeball from exposure and treat the underlying disease.
Graphical Abstract
Keywords
Main Subjects
Introduction
Pemphigus, derived from the Greek word "pemphix," meaning bubble or blister, is a rare group of autoimmune, intraepidermal blistering diseases affecting the skin and mucous membranes. This group encompasses five primary variants: pemphigus vulgaris (PV), pemphigus foliaceus (PF), pemphigus erythematosus, drug-induced pemphigus, and paraneoplastic pemphigus. Pemphigus vulgaris is the most common form of pemphigus, which accounts for at least three-quarters of all cases. It is a serious mucocutaneous autoimmune disorder affecting intraepidermal cell cohesion, resulting in the formation of flaccid blisters and painful erosions [1-3].
The prevalence of PV varies globally. In Europe and North America, 65-90% of pemphigus cases are attributed to PV. Data from the Danish National Patient Registry indicates a prevalence of pemphigus at 60 per one million population in 2006, while based on German Health Insurance, the prevalence of pemphigus was 148 cases per one million population in 2014 and 53 cases per one million children and/or adults in 2015. Pemphigus patients are most commonly diagnosed between the ages of 45 and 65 [4]. At Sanglah Hospital, Bali, out of 33 pemphigus patients, 26 (78.78%) were diagnosed with pemphigus vulgaris [5].
Ectropion is characterized by the malposition of the eyelid margin, manifesting as an outward folding of the eyelid margin [6-8]. Cicatricial ectropion results from scar tissue causing shortening of the anterior lamella of the palpebra, leading to an imbalance between the anterior and posterior lamellae, pulling the eyelid margin away from the eyeball [9,10].
Cicatricial ectropion can arise from various causes, including burns, chemical and mechanical trauma, iatrogenic factors, and chronic inflammation such as lamellar ichthyosis and pemphigus vulgaris. If scar tissue forms in the anterior lamella, it may result in the shortening of the anterior lamella, leading to complications such as dry eye syndrome, exposure keratopathy, infection, blindness, and even eyeball perforation [6-9,11].
Considering that pemphigus vulgaris is an uncommon condition associated with cicatricial ectropion, the authors find it imperative to present this case. This case report aims to contribute to the knowledge of ophthalmologists regarding this disease. Case Illustration
A 61-year-old man was referred from a dermatovenereology clinic with the chief complaint of the right inferior palpebra being pulled down for the past two months. This complaint developed gradually, with the lower right palpebra progressively descending over time. The patient reported the ability to close the right palpebra perfectly. While experiencing watery eyes, there were no complaints of blurred vision, pain, dry eyes, foreign body sensation, or burning sensation in the right eye.
Initially, the patient complained of bullae in the oral cavity 1.5 years ago, which later enlarged, ruptured, and extended throughout the entire oral cavity. Six months ago, bullae appeared in the chest area, and they subsequently enlarged and ruptured, spreading to the chest, neck, stomach, back, and face. The patient reported that the bullae appeared suddenly, accompanied by pain in the affected areas. The patient was referred from the dermatovenereology clinic with a diagnosis of pemphigus vulgaris.
The patient mentioned that he had never experienced such symptoms before. He denied a history of hypertension and diabetes mellitus. There is no reported history of allergies, smoking, trauma, or surgery. In addition, there is no known family member who has experienced a similar disease.
During his initial visit examination at the eye clinic, his visual acuity in the right eye was 5/6 with a correction of C-0.50 A110, improving to 5/5, and in the left eye, it was 5/12 with a correction of C-1.25 A90, also improving to 5/5. The intraocular pressure for both the right and left eyes was recorded at 17.3 mmHg. The inspection examination of the anterior segment of the right eye revealed ectropion, an everted inferior punctum, madarosis, 1 mm lagophthalmos (Figure 1), scleral show, a good bell's phenomenon, clear cornea, negative fluorescein test, no conjunctival hyperemia, and other parameters within normal limits. In contrast, the anterior segment of the left eye was within normal limits (Figure 2). The palpation examination of the right inferior palpebra showed that ectropion did not resolve during the 2-finger test, with a lid distraction of 8 mm based on the distraction test (Figure 3). The inferior palpebra did not return to its anatomical position even though the patient blinked during the snap-back test. The posterior segment examination of both eyes revealed a positive fundus reflex, a sharp margin of the optic nerve head, normal color, no retinal hemorrhage, no exudate, and positive macular reflex.
During the examination in the dermatovenereology clinic, erythematous macula with a sharp border, erosion with a clean base, and some covered in reddish-brown crusts were observed at the right periorbital region (Figure 1). Erythematous macula with a sharp border, erosion with an erythema base covered with yellow crusts surrounded by areas of hypopigmentation, was noted at the corner of the mouth (Figure 4A). Alopecia areata with hypopigmentation, some brownish-red crust, and squama were present at the right temporalis (Figure 4B). At the posterior neck, a hyperpigmentation macula with a sharp border, some erosion with a clean base, and no crust were observed (Figure 4C). In the oral cavity, erosion with a clean base and a thick white plaque with a sharp border were seen at the labia, and there was no erosion on the tongue (Figure 4D, E, and F). Diffuse erythematous macula with erosion, clean base, no crust, and some hyperpigmentation macula with a sharp border were found at the anterior thorax and abdomen (Figure 4G). At the posterior thorax, multiple hyperpigmentation macula with a sharp border and hypopigmentation at the center were present (Figure 4H). There was also an erythematous macula with a sharp border, erosion, clean base, and necrotic tissue at the right elbow (Figure 4I).
According to the blood test examination, the results were within normal limits. The patient underwent candida testing by a dermatologist with negative results. The patient was diagnosed with cicatricial ectropion of the inferior palpebra in the right eye (Oculus Dextra or OD) caused by pemphigus vulgaris. At the eye clinic, the patient received treatment, including chloramphenicol eye ointment every eight hours and Lyteers eye drops, 1 drop every 4 hours. In the dermatovenereology clinic, the patient has been prescribed prednisone (5 mg tablet, two tablets every eight hours), natrium fusidate ointment every 12 hours, vaselin album every 12 hours for dry skin, mefenamic acid tablets every 8 hours, and clobetasol propionate 0.05% cream every 12 hours to be applied to the skin lesions and periorbital skin.
Discussion
Cicatricial ectropion, characterized by the outward rotation of the eyelid margin, is primarily caused by the shortening of the anterior lamella due to scar tissue. This shortening leads to the eyelid margin moving away from the eyeball. This condition can be associated with various factors, including chronic actinic skin damage, congenital influences, various forms of trauma (mechanical, chemical, and thermal), cicatrizing skin tumors, drugs, allergies, involutional changes, and chronic skin inflammation [6-9,12]. In the case of this patient, the outward rotation of the eyelid margin is a result of scar tissue formation due to chronic inflammation in the right inferior periorbital area caused by pemphigus vulgaris.
Typically, ectropion patients present complaints such as watery eyes, eye irritation, and cosmetic concerns. This particular patient is experiencing watery eyes, which is attributed to the eversion and drying of the inferior punctum. This can lead to stenosis, resulting in epiphora. Epiphora is further compounded by an inadequate tear pump mechanism and reflex tearing induced by exposure. Eye irritation is another common complaint and arises from the uneven distribution of the tear film and exposure of the conjunctiva and cornea [8-10,13]. Notably, this patient does not report irritation in the right eye. This absence of irritation is explained by the patient's ability to close the right superior palpebra despite the presence of 1 mm lagophthalmos. In addition, the bells phenomenon of the right eye is reported to be good.
During palpation, a 2-finger test can be conducted to assess the presence of palpebral retraction. In this examination, two fingers are placed on the skin of the palpebra, and the palpebra is gently elevated superiorly. This maneuver allows for the evaluation of additional skin on the anterior lamella. If the palpebra move superiorly and the retraction improves, the likely cause of the retraction is anterior lamella deficiency. Conversely, if the palpebra does not move and retraction persists, it suggests that the retraction is caused by scar tissue in the posterior or middle lamellae. At the time of the 2-finger test, the ectropion of the right inferior palpebra did not improve, indicating the possibility that, in addition to anterior lamella involvement, scar tissue may also be present in the middle lamella [11].
In some cases, a combination of lid laxity along with shortening of the lamellae exists. Inferior lid laxity can be assessed through the distraction test and snap-back test. In the distraction test, the palpebra are pulled anteriorly away from the eyeball and measured with a millimeter ruler. If the measurement exceeds 6 mm, it indicates weakness in the palpebra. The snap-back test involves pulling the inferior palpebra away from the eyeball, releasing it, and observing how quickly the palpebra return to their normal position without blinking. In patients with lid laxity, the lids may return slowly or not at all. Severe weakness may result in the palpebra not returning to their normal position, even with blinking. If the palpebra do not return to the normal position, it indicates poor tone of the orbicularis oculi muscle [7-8,10-11,14]. In the case of this patient, the distraction test resulted in a lid distraction of 8 mm, and despite blinking, the palpebra did not return to their normal position. This examination suggests that the right inferior palpebra has laxity.
Pemphigus vulgaris (PV) is an autoimmune reaction involving IgG antibodies against desmoglein 3 (Dsg 3) and Dsg 1, clinically manifested by bullous eruptions on the skin and mucous membranes. It primarily affects older patients, with a median onset age of 71 years [15,16]. This particular patient started developing blisters in the oral cavity at the age of 60 years.
Autoantibodies, specifically IgG4 and IgG1, react with antigens such as Dsg3, Dsg1, and desmocollins, which are present in desmosomes. Desmosomes are components of keratinocytes that bind neighboring cells. As a result of this autoimmune reaction, basal keratinocytes become separated from the basement membrane and neighboring keratinocytes, giving rise to the characteristic appearance known as a 'row of tombstones.' This process induces plasminogen activator and activates complements, ultimately leading to epidermal acantholysis [15,16].
The hallmark of the disease is the presence of flaccid bullae. The disease can manifest as localized or extensive, with blisters appearing on the skin or mucosa, often affecting both. Painful oral erosions typically precede the onset of skin blisters in weeks or months. Almost all patients experience the involvement of mucous membranes, with the oral mucosa being the most commonly affected site, although other areas, such as the conjunctiva, pharynx, and genital mucosa, are also frequently involved. Nonpruritic flaccid blisters, varying in size from 1 cm to several centimeters, gradually appear on normal or erythematous skin and may be localized for a considerable time. Common sites for these blisters include the scalp, face, upper trunk, axillae, and intertriginous zones. The blisters easily rupture due to the fragile vesicle roof, which consists of only a thin portion of the upper epidermis. After rupture, many patients develop crusted erosions in the areas where the blisters were present [2,15-16]. In the described case, the patient initially developed blisters in the oral cavity, followed by the appearance of blisters on the skin of the abdomen and chest after six months. Two months ago, blisters appeared on the neck, face, and right temporal area, which enlarged, ruptured easily and were subsequently covered by crusts.
The management of cicatricial ectropion involves both medical and surgical approaches. In medical management, symptomatic therapy, such as eye drops and ointments for lubrication, can be provided. It is crucial to identify dermatological disorders contributing to cicatricial ectropion that may be treatable through medical means alone. For the treatment of pemphigus vulgaris, systemic corticosteroids are often necessary, especially in more widespread cases. Prednisolone is typically prescribed at a dose of 0.5-1.5 mg/kg or higher, depending on the extent of the disease, rate of progression, clinical response, and overall patient condition. Resistant and severe cases may require very high doses, such as prednisolone 60-180 mg/day. These doses work by upregulating the expression of desmoglein molecules on the surfaces of keratinocytes, among other anti-inflammatory effects. The dosage is gradually reduced when new blisters cease to appear. Mild cases of pemphigus vulgaris or pemphigus foliaceus may respond to clobetasol propionate 0.05% cream applied to mucosal and skin lesions twice a day for at least 15 days, followed by a progressive taper [3,8-9,16]. In the case of this patient, the management included chloramphenicol eye ointment every 8 hours, artificial tears eye drops every 4 hours to avoid eyeball exposure, prednisone tablets 5 mg (2 tablets every 8 hours) for inflammation reduction, natrium fusidate ointment every 12 hours, vaselin album every 12 hours to moisten the wound, mefenamic acid tablets every 8 hours, and clobetasol propionate 0.05% cream applied to skin lesions and periorbital skin every 12 hours.
Conclusion
Pemphigus vulgaris is an autoimmune disease characterized by widespread bullous eruptions. Chronic inflammation in the periorbital region can lead to the formation of scar tissue in the anterior lamella, resulting in ectropion. The management of this condition is focused on protecting the eyeball from exposure and addressing the underlying autoimmune disease.
Acknowledgments
We express our gratitude to Ratna Doemilah, Dr. Sp.M(K) for her valuable suggestions regarding the comprehensive diagnosis and treatment of ectropion in this patient. Special thanks to Dr. Trisniartami, Dr. Sp.KK(K) for the support and insightful discussions on pemphigus vulgaris. We acknowledge that this case report would not have been possible without the cooperation and contributions of all parties involved.
Funding
No funding was received for this study.
Authors' Contributions
Examine and treat the patient, H.H., R.D., T.S.; conceptualization, H.H.; prepared and wrote the original draft, H.H.; correction the draft, R.D., T.S.; editing, H.H.; supervision, R.D., T.S.. All authors have read and agreed to the published version of the manuscript.
Conflict of Interest
There is no conflict of interest in this study.
Orcid:
Henu Hadiyantama*: https://orcid.org/0009-0005-3463-1489
Ratna Doemilah: https://orcid.org/0009-0007-4399-6986
Trisniartami Setyaningrum: https://orcid.org/0000-0002-6923-7167
----------------------------------------------------------------------------------------
How to cite this article: Henu Hadiyantama*, Ratna Doemilah, Trisniartami Setyaningrum, Comprehensive diagnosis and treatment of cicatricial ectropion caused by pemphigus vulgaris. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(6), 731-738. Link: https://jmpcr.samipubco.com/article_188440.html
----------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
