Document Type : Original Research Article
Authors
- Iriana Wahyu Nasifah 1
- Damayanti Tinduh 2
- Indrayuni Lukitra Wardhani 2
- Paulus Sugianto 3
- Soenarnatalina Melaniani 4
1 Physical Medicine and Rehabilitation Residency Program, Department of Physical Medicine and Rehabilitation, Faculty of Medicine, Airlangga University, Dr Soetomo General Academic Hospital, Surabaya, Indonesia, 60264
2 Department of Physical Medicine and Rehabilitation, Faculty of Medicine, Airlangga University - Dr. Soetomo General Academic Hospital, Surabaya, Indonesia, 60264
3 Department of Neurology, Dr. Soetomo General Academic Hospital, Faculty of Medicine Airlangga University, Surabaya, Indonesia, 60264
4 Department of Epidemiology, Biostatistics, Population Studies, and Health Promotion, Faculty of Public Health, Airlangga University, Surabaya, Indonesia, 60264
Abstract
Frailty syndrome is a syndrome in geriatrics characterized by reduced functional ability and adaptive function resulting from degradation of the function of various systems in the body, as well as increased vulnerability to various types of pressure (stressors) and ultimately reduced functional performance. The study subjects were 38 elderly people with frailty syndrome. Participants in both groups were required to take part in conventional exercises programmed by the Nursing Home 5-7x/week for ±15 minutes. The outcomes assessed were static and dynamic balance function by measuring the one leg stance (OLS) and timed up and go (TUG) tests at baseline (pre-test) and after 4 weeks of intervention (post-test). There was a significant increase in the OLS test and a significant decrease in the TUG test in the intervention group (right OLS test p=0.016; left OLS test p=0.001 and TUG test p=0.001). In the control group, there were no significant changes in the OLS test and TUG test (right OLS test p=0.368; left OLS test p=0.157 and TUG test p=0.297). Changes in the right and left OLS tests between groups showed significant results between the pre-test and post-test between groups (p=0.005 and p=0.001). Changes in the TUG test between groups showed significant results in the pre-test and post-test between groups (p=0.004). The addition of multicomponent Vivifrail training for 4 weeks in elderly people with frailty syndrome can improve static balance function as measured by the OLS test and dynamic balance function as measured by the TUG test.
Graphical Abstract
Keywords
Main Subjects
Introduction
Frailty syndrome is a syndrome in geriatrics characterized by decreased functional ability and adaptive function caused by the functional degradation of various systems in the body, as well as increased vulnerability to various types of pressure (stressors) and ultimately reduced functional performance. Research on 111 men and women aged over 75 years with frailty said they were 3.6 times more likely to fall than those without frailty [1,2]. Various analyses have identified numerous predictors associated with the increased risk of falls in elderly individuals with frailty syndrome. One of the main problems with increasing the risk of falls is the presence of balance disorders [2,3].The aging process disrupts the function of postural control components. Decreased strength is associated with decreased postural control, and impaired postural control is associated with increased risk of falls [4].
Handling frailty syndrome requires multidimensional treatment, one of the main interventions in preventing and treating frailty conditions, among other physical exercises, is multicomponent exercise. The recommended multicomponent exercise includes strengthening, endurance, balance training and flexibility exercise [3].
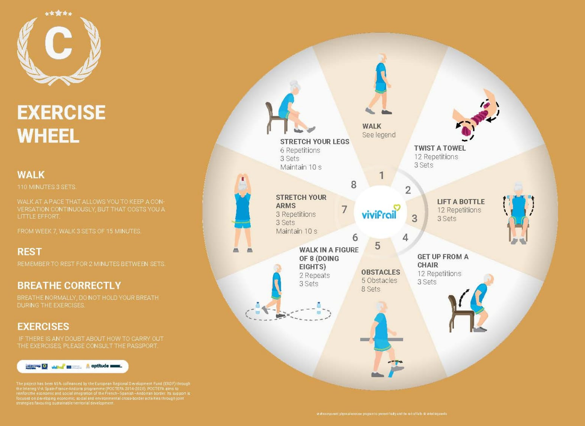
Handling frailty syndrome physical exercise in the form of multicomponent exercises that can improve statistical and dynamic balance function. A multicomponent exercise that has balance, strengthening, endurance, and flexibility components is the Vivifrail exercise. The Vivifrail program is an exercise in frailty syndrome developed in Europe (European Union's Erasmus+ program) [5]
Currently, there are few studies that objectively measure the effects of Vivifrail multicomponent exercise on static and dynamic balance function, especially for Asian communities, especially Indonesia. A decrease in balance function will affect the risk of falls, ambulation function, decreased walking speed, and decreased activity level, easy fatigue, which ends in a decrease in functional capacity and quality of life of the elderly. Currently, there are various kinds of physical exercises carried out in elderly groups and in nursing homes. Conventional physical exercises performed by the elderly, especially in Surabaya, do not yet refer to standardized, evidence-based recommended exercises. Therefore, the authors are interested in further examining the effect of adding Vivifrail multicomponent exercises to conventional exercises on static and dynamic balance in subjects with frailty syndrome.
Method
Subjects
Ethical approval was provided by the Ethical Committee of Soetomo General Academic Hospital Surabaya with number 11/EC/KEPK/2023. The subject of this study is elderly people aged > 60 years with frailty syndrome who meet the inclusion criteria and do not meet the exclusion criteria who live in Griya Wreda Jambangan, Ketintang Madya St. VI No. 15a Jambangan Surabaya. Sampling was carried out using proportional random sample. Inclusion Criteria: 1) Elderly aged ≥ 60 years, 2) have at least 1 of 5 SF phenotypes according to the criteria of Fried et al. (2021) [6]. 3) undergo to ambulate independently with or without a walking aid with a Barthel Index ≥60; 4) good vision and hearing function; 5) there is no decline in cognitive function so that subjects can understand and follow instructions well (MoCa-Ina score≥26); 6) stable hemodynamics; and 7) subjects are willing to take part in the research program by filling out an informed consent form.
Exclusion criteria included having factors that impeded the performance of the physical exercise program and testing procedures as prescribed by the physician. These factors refer to the Vivifrail program implementation guidelines [6]:
1) History of cardiorespiratory disease that affects physical performance during exercise (NYHA class 3-4 heart failure, COPD, acute heart attack, unstable angina, uncontrolled arrhythmia, aneurysm, severe aortic stenosis, acute endocarditis/pericarditis, and acute or severe respiratory failure); 2) blood pressure (>180/100mmHg); 3) uncontrolled postural hypotension; 4) acute thromboembolism of lower extremities; 5) have a history of fracture in the last 3 months or more than 3 months but not union as proven by X-Ray; 6) Suffering from an infectious disease that can affect the general condition and implementation of training; 7) have other conditions that cause moderate to severe functional limitations (Barthel index <60); 8) suffering from muscle pain and lower limb joint pain with WBFS (Wong Baker Face Scale) ≥ 4 and clinical signs of swelling, redness and warmth to the touch; 9) chronic diseases that interfere with the mobility function of the elderly (ambulatory disorders due to stroke, uncontrolled diabetes and balance disorders due to intracranial and extracranial processes such as BPPV and other neurological disorders that can disrupt balance); 10) and have received special physical training using methods other than the routine program at a nursing home in the last 3 months. Drop Out Criteria: 1) The subject withdraws; 2) the subject is not present for two consecutive meetings; 3) attendance is less than 90% of the total attendance attended; and 4) the subject is sick, so he has to stop the exercise program; 5) Died. This study used a true experimental method with a pre- and post-test randomized control group design. Elderly subjects who have met the inclusion and exclusion criteria screening are then carried out SPPB assessment and fall risk assessment according to the Vivifrail protocol. Data collection on subject characteristics (name and age), subjective examination (history taking), and physical examination, and also other examinations needed to determine the inclusion and exclusion criteria were carried out by the researcher 1 week before the research intervention was carried out. All data were recorded on the data collection sheet. Furthermore, randomization was carried out. Subjects were asked to follow Vivifrail Exercise according to the exercise category allocated based on the SPPB results and fall risk assessment. At the beginning, one introductory session will be conducted to condition the participants for the exercise intervention and to provide guidance for patients to be more familiar with the movements that will be performed during the Vivifrail exercise before the intervention training session is implemented. In this session, participants will also be given information in the form of a short video and guidance sheet and given the opportunity to consult about the Vivifrail exercise program and the research series.
The intervention exercise session program will be conducted 5 times per week for 4 weeks according to the daily exercise menu in the programmed Vivifrail passport. For the safety of the subjects and proper execution of the exercises, the exercises will be supervised by 2-3 nurses, 5 social workers, and 5 doctors.
Participants in both groups are required to follow conventional exercises programmed by nursing home in the form of a combination of light intensity aerobic activities and physical stretching 5-7x/week for 10-15 minutes which are divided into components of 5 minutes of warm-up, 5 minutes of core, and 5 minutes of cooling. Participants' attendance will be recorded and the implementation of this conventional exercise fully follows the existing exercise protocol at Surabaya nursing home. The final measurement in both groups will be carried out within a maximum of 1 week after the subject completes the last exercise. The collected data will then be analyzed in accordance with the research objectives.
Statistical analysis
The data obtained will be input and processed using the SPSS 20.0 for Windows™ program. A descriptive data presentation was carried out to determine the characteristics of all data. Test data normality using the Shapiro-Wilk test. A parametric statistical test is carried out if the data is normally distributed. To test the comparison between before and after treatment in each group, use the paired sample t-test if the data is normally distributed; if the data is not normally distributed, then use the Wilcoxon rank sign test, and then to compare the difference between the treatment and control groups, the unpaired should be used t-test if the data is normally distributed; if the data is not normally distributed, the Mann-Whitney test should be utilized.
Results
The characteristics of the study subjects, as well as normality and homogeneity data on the characteristics of the subjects in the intervention group and the control group, are shown in Table 1. Comparison of OLS Test before and after treatment in Intervention Group are presented in Table 2 and the comparison of dynamic balance (TUG) right and left before and after treatment in the Intervention Group i is summarized in Table 3. Comparison of static balance (OLS) right and left before and after treatment in the Control Group is indicated in Table 4. Comparison of dynamic balance (TUG) right and left before and after treatment in the Control Group is presented in Table 5.
The difference in improvement of static balance values (OLS) between Intervention and Control Groups is provided in Table 6. Difference in improvement of dynamic balance (TUG) values between Intervention and Control Groups is listed in Table 7.
Discussion
Balance is a general term that describes the dynamics of body posture to prevent falls. Balance is required to maintain position, remain stable while moving from one position to another, perform activities of daily living, and move freely in the community. Age, weight, and BMI contribute to postural instability. In a study conducted by R. Mohammed et al. found that there was a significant correlation between age and balance performance [7]. Age-related physiological changes, as documented in studies such as, encompass a spectrum of alterations including decreased nerve conduction velocity, diminished muscle strength, and heightened tissue stiffness. These factors collectively contribute to the overall decline in balance and postural stability observed in aging individuals. Men and women as they age are found to have decreased balance performance, it is reported that women consistently have worse performance than men [8]. In the study of R. Mohammed et al. reported significant differences in balance performance between men and women [7]. In this study, the age characteristics of the intervention and control groups were considered homogeneous so that the age variable did not confuse the OLS and TUG test values obtained. Similarly, the composition of height, weight and body mass index is a factor that affects the value of the OLS and TUG tests. In this study, the characteristics of height, weight, and BMI in the treatment and control groups were homogeneous with p>0.05.
The frailty category was also assessed in the basic characteristics of the population targeted by this study. The total subjects who participated in this study were mostly with frailty syndrome in the pre-frailty category with a total of 34 people (89.47%) while the frailty category was 4 people (10.53%). The intervention group had a total of 16 participants with the pre-frailty category (84.2%) while frailty was 3 people (15.8%). The control group had 18 participants with pre-failty category (94.7%) while frailty was 1 person (5.3%). Subjects in the intervention group and control group in this study had a proportion of participants with frailty categories that were not much different between groups.
Impaired balance function can be affected by the fear of falling as assessed by the FES-I. The fear of falling affects the restriction of daily activities, as well as the limited willingness to perform exercises. This is prone to postural instability and deconditioning-related muscle weakness [9]. Subjects in the intervention group and control group in this study had a proportion of participants with fear of falling categories that did not differ much between groups.
Assessment of the functional capacity of the elderly is measured using the Short Physical Performance Battery (SPPB) score. Low SPPB scores and slower walking speeds will affect balance performance in the elderly [10]. In this study, the baseline data of the average 6m walking speed in the intervention group and control group did not differ significantly (p>0.05). Similarly, the SPPB values at screening in both groups were normally distributed (p>0.05). This homogeneity analysis of subject characteristics eliminated the possibility of bias by confounding characteristic variables in the acquisition of OLS and TUG test scores, which were the dependent variables in this study.
The results of this study showed the addition of Vivifrail multicomponent training to conventional training for 4 weeks was able to improve static balance function in the elderly examined using the right and left OLS tests with open eyes (p = 0.001 and p = 0.001). Post-intervention changes in the right and left OLS tests in the intervention group had effect sizes of 0.559 and 1.103 indicating that the 4-week Vivifrail multicomponent exercise program provided a moderate to large effect on improving the static balance function of both limbs.
The provision of Vivifrail exercises to the elderly population in this study followed the exercise categorization protocol based on SPPB scores and the risk of falling. The intervention group participants were divided into 3 exercise groups, namely category C, C + E, and D. Of the 19 subjects of this study, category C was 4 people (21%), category C + E was 4 people (21%), and category D was 11 people (58%). Vivifrail's multicomponent exercise prescription refers to the exercise protocol developed by Izquierdo et al. in 2017. Flexibility, balance and cardiovascular exercise components in Vivifrail are the dominant components programmed 5 times per week while strengthening exercises are programmed 3 times per week with a total duration of 30-60 minutes. Each stretch should be performed for 10-30 seconds, until it feels slightly uncomfortable. Multicomponent exercise in the elderly can affect neuromuscular adaptation with increased motor control which is closely related to the balance process. Balance training can optimize the function of sensory input, cognitive and musculoskeletal control. In addition, upper and lower limb strengthening exercises can improve blood circulation and skeletal muscle metabolism which can affect the remodeling process in the form of changes in muscle mass and volume. Endurance/aerobic training stimulates mitochondrial biogenesis, increasing muscle oxidative capacity. Flexibility training also maintains joint range of motion. The effect of multicomponent training is very supportive of improving the static balance function ability of the elderly with frailty syndrome [11-13].
Until now there has been no research on the assessment of static balance with the OLS test after the provision of a multicomponent exercise program specifically in the elderly with frailty syndrome. Balance checks carried out in the SPPB component include the first position, the subject stands with both feet parallel opened shoulder-width apart, the second position, the subject stands with semitandem legs, and the third position, the subject stands with tandem legs. In line with the results of our study, in a study conducted by Cuenca-Zaldivar et al. (2022) which aims to evaluate the effect of Vivifrail multicomponent exercise performed daily, 40 minutes per session, for 3 weeks in elderly frailty post COVID-19 with an average age of 73 years with a total of 101 elderly subjects, obtained static balance function with Romberg's test examination, semitandem and tandem obtained significant results (p<0.001) [14].
Another study showed similar results in terms of significant improvement in static balance function in the OLS test (p=0.001) in elderly people with stage 1 locomotive syndrome, with an average age of 75 years, living in nursing homes. The intervention was locomotor exercise combined with aerobic exercise for 8 weeks. This improvement was suspected to be an increase in serum Brain Derived Nerve-growth Factor (BDNF) in the elderly who underwent multimodal exercise. The increase in serum BDNF protein triggered by exercise is closely related to the process of neuroplasticity. The appearance of BDNF when the elderly do multimodal exercise can stimulate motor responses so that it can stimulate the excitability of motor networks in the spinal cord, modulate the release of acetylcholine at neuromuscular synapses, maintain the level of neuron resistance so that it has the potential to increase neuron growth and trigger neuroplasticity, to improve static balance function [15-17].
In an elderly population with knee osteoarthritis who received multicomponent exercise performed twice a week at moderate intensity. The physical exercise incorporated functional training and walking. Results showed that MCEP for 6 months was able to improve patients' OLS and mobility (walking speed) (Coelho-Júnior et al., 2018). A systematic review study on ambulatory older adults in the community also showed that a physical exercise program involving a lower extremity strengthening exercise component showed significant effects on lower extremity strength, balance (including OLS), and mobility [18].
The results of this study showed that the addition of Vivifrail multicomponent training to conventional training for 4 weeks was able to improve dynamic balance function in the elderly examined using the TUG test (p = 0.001). Post-intervention changes on the TUG in the intervention group had an effect size of 1.230 which indicates that the Vivifrail multicomponent exercise program for 4 weeks provided has a large effect on improving the dynamic balance function of the elderly with frailty syndrome.
The Vivifrail multicomponent exercise protocol includes intensive flexibility, balance, strengthening, and cardiovascular exercises 5 times per week with an increase in intensity every 2 weeks. Another 4-week study with Vivifrail in Spain on frail elderly living in assisted living facilities in Spain also found an improvement in Timed Up-and-Go scores in the intervention group with 11.2% faster time recorded (p = 0.004, effect size=0.35). It was also reported that 6 out of 9 participants who started the exercise with pre-frailty status (66.7%) were able to upgrade to robust after the intervention [10]. TUG values, in addition to describing dynamic balance, can also be used to signify functional and ability a predictor of falls [2-3,19]. These improvements are positive for reducing fall risk and fear of falling in general for older adults across the frailty spectrum [20,21].
Studies with similar methods and durations of Vivifrail exercise have also obtained results consistent with this study [22]. They assessed the impact of a 4-week customized multicomponent exercise program on functional capacity and muscle strength in sarcopenia elderly and showed significantly shorter TUGs (-4.2 seconds, p<0.001) after 4 weeks. However, after 14 weeks of COVID-19 isolation without physical exercise, these improvements in dynamic balance were not maintained and almost returned to baseline values as without exercise. This report suggests that to prevent significant functional decline in the elderly, an intervention of at least 4 weeks, 3 times per year (avoiding more than 14 weeks of inactivity between exercise periods) would be decisive.
Another multicomponent study on elderly with frailty syndrome in Thailand also supported the results of this study. Multicomponent exercise by combining instructor-guided exercise with home-based independent exercise conducted for 24 weeks found that there was an acceleration of TUG time after 12 weeks to 24 weeks of exercise (from 12.21 ± 2.26 to 10.33 ± 2.9) p<0.01 [23].
Balance training can optimize sensory input, cognition, and musculoskeletal control. In addition, upper and lower extremity strengthening exercises can improve blood circulation and skeletal muscle metabolism, thereby influencing the remodeling process in the form of changes in muscle mass and volume. Endurance/aerobic exercise stimulates mitochondrial biogenesis, thereby increasing muscle oxidative capacity. Flexibility training also maintains joint range of motion. The effects of multicomponent training are beneficial in improving dynamic balance function in the elderly with frailty syndrome.
Dynamic balance function with the TUG test has improved after multicomponent exercise in the elderly which routinely stimulates the mechanics of the body so as to increase the production of neurotrophoic factor (BDNF) which is related to the process of neurogenesis. The existence of the neurogenesis process, the number of nerve fibers as well as afferent and efferent impulses increases the dynamic balance function of the elderly can improve [16,17].
In the study Romero-García et al. multicomponent exercise intervention for 12 weeks, in the elderly aged 65-80 years, with the control group getting treatment to continue daily physical activities such as yoga, tai chi, and cardio-dance with a frequency of exercise at least 3 times per week. The statistical test results obtained in the control group were not significant in static balance function after 12 weeks (p=0.16). The control group also experienced a decrease in functional capacity results [24].
A systematic review and meta-analysis aimed to analyze the effect of different types of exercise such as aerobic, resistance, multicomponent, and balance training on static balance in a healthy elderly population. The systematic review summarized findings from a total of eight studies and included a total of 335 participants. The review showed that interventions based on different types of exercise improved static balance in the elderly population, but without statistically significant differences compared to the control group [25].
The control group did not experience an increase in the right and left OLS test values after 4 weeks of observation. Conventional exercises performed by the control and intervention groups were routine exercises programmed by the nursing home. This conventional exercise consists of low-intensity aerobic exercise and stretching exercises with a duration of 10-15 minutes per day every day. Conventional exercise is considered to still not fulfill the exercise prescription for elderly with frailty. Specifically for older adults at risk of falls, ACSM recommends performing balance training 3 or more days per week and considering participating in standard fall prevention programs [6,26]. Conventional training does not have a balance and strength training component, thus affecting the static balance function value with the OLS test as shown by the absence of significant improvement in static balance function at the beginning and end of the 4-week training session in the control group.
The results obtained in the control group of this study did not show a significant change in TUG time before compared to after receiving conventional exercise for 4 weeks (p=0.297, p>0.05) with a small effect size (0.247). The conventional exercise provided in order to increase the physical activity of the elderly consists of aerobic exercise and flexibility exercises performed for approximately 15 minutes. The components of this conventional exercise that do not have specific components for balance training and walking pattern training may affect the results of the study in the control group which are not significant. The aerobic and flexibility exercise components with a short duration in the conventional exercise program for 4 weeks have not been able to improve dynamic balance (through the TUG test) in the elderly with frailty syndrome. This shows the importance of doing multi-component exercises for the elderly adequately, regularly, and continuously.
Romero-García et al. (2021) study on the elderly aged 65-80 years, with a multicomponent exercise intervention for 12 weeks, with the control group getting treatment to continue daily physical activities such as yoga, tai chi and cardio-dance with a frequency of exercise at least 3 times per week. In the control group that received the TUG test, there was no improvement in the initial median result of 9.72 seconds and after 12 weeks of multicomponent training the median value was 11.40. Overall, the control group experienced a decrease in functional capacity results [24].
In this study, it was found that the magnitude of changes in the right and left OLS tests in the intervention group and control group was found to be significant, with right delta OLS p=0.024 and left delta OLS p=0.001. In the intervention group, delta OLS before and after training has increased, right limb OLS of 4.87± 8.71 seconds and left limb OLS of 7.21 + 7.11 seconds. The effect size values of the right and left OLS test deltas after the intervention between groups in this study were 0.766 and 1.323, indicating a moderate to large effect. These results indicate that the addition of Vivifrail exercise for 4 weeks in the elderly with frailty syndrome can improve static balance function compared to conventional exercise.
The results of this study are in line with previous research which states that multicomponent training consisting of balance, resistance, endurance, and flexibility exercise provides significant results in both balance and strength improvement at 12 weeks and 14 weeks of multicomponent training intervention (p<0.001). The improvement in balance in the intervention group may be due to joints that are stimulated by proprioceptors that can affect stability. Improved balance function will improve physical function and increase activity levels [23]. Previous research mentions that multicomponent exercise programs improve balance, and strength in the elderly, especially with frailty, and should consist of resistance, strength, and balance exercises. Another reason why balance is positively correlated with muscle strength [27].
The results of this study showed a significant improvement in the right and left OLS of the intervention group, but had not reached the minimum detectable change (MDC) commonly used for OLS evaluation. The minimum detectable change that is considered a real change is more than 24.1 seconds [28]. This could be influenced by the relatively short time of implementation of the intervention in this study, which was 4 weeks. The achievement of an increase in the value of the change in OLS time in this study is around 50% of the MDC, which indicates that the addition of static balance has occurred, but it still requires training with a longer program duration so that changes can be considered clinically meaningful.
In the control group, there was a decrease in the right and left OLS values after 4 weeks of conventional training only. There was a decrease in right OLS of -1.31±7.39 seconds and left OLS of -2.40±7.40 seconds. A longitudinal intervention study in an elderly population in Japan also observed a similar phenomenon, where over 12 months of observation in the control group there was a trend towards decreased function, not only static balance (from the OLS test), but also muscle strength, walking speed, and 6-minute walking distance [20]. This may be due to the ongoing degeneration process in the elderly. In particular, age-related vulnerability syndromes lead to decreased biological adaptability, due to degeneration of physiological system regulation, which puts individuals at risk, especially when faced with mild to severe levels of stress. This leads to worse outcomes in terms of disability, hospitalization, and mortality [29,30].
In this study, it was found that the magnitude of change in TUG test in the intervention group and control group was found to be significant, with delta TUG p=0.007. The effect size value of the TUG test delta in this study was 0.921, indicating a large effect of the addition of Vivifrail exercise and conventional exercise in the intervention group.
In the intervention group, there was a decrease in TUG time of -1.46±1.19 seconds. The delta TUG value studied in previous studies suggested a clinically meaningful MDC for the TUG test of 2.08 seconds (Donoghue et al., 2019).. In this study, there were 6 out of 19 participants (31.6%) in the intervention group who experienced a decrease in TUG time of more than 2.08 seconds. These results indicate that the addition of Vivifrail exercise for 4 weeks in elderly with frailty syndrome has a positive impact on improving dynamic balance function.
A study in an elderly Spanish population that followed the Vivifrail program for 3 weeks reported the efficacy of Vivifrail exercises in improving general condition in post-COVID-19 elderly after intensive care unit. There was a reduction in mean TUG time by 8 seconds (p<0.001). Furthermore, only less than 2% of patients showed an adverse response at the end of the program and none of them discontinued the program due to any adverse effects, so Vivifrail has the necessary safety to be applied to post-COVID-19 elderly patients, and the cost is low [31].
A number of studies have investigated the relationship between frailty and fall risk in older people [2,30,32]. Fall risk assessment according to the Vivifrail protocol: cumulative number of falls in the past year, cumulative number of falls with physician care, suffered at least 1 fall in the past year and TUG [6].
In this study, the addition of Vivifrail multicomponent exercise for 4 weeks was given to elderly people with frailty syndrome in Jambangan nursing home, Surabaya. Static balance function assessed by OLS test before and after the Vivifrail exercise obtained results that showed significant improvement when compared to the control group. In addition, the large impact size supports the superiority of this exercise in improving cardiorespiratory fitness in the elderly with frailty syndrome in a fairly short period of 4 weeks.
In addition, the static balance function assessed by the TUG test before and after training was compared, with the results showing significant improvement in the group that received Vivifrail training with a large impact force. This is a strong basis that supports the implementation of the use of Vivifrail in the elderly with frailty syndrome who generally often complain of dynamic balance problems. Hopefully, with the improvement of dynamic balance function, the elderly will become more active, fit, and independent.
The provision of the Vivifrail exercise program for the elderly is adjusted to their respective functional levels by doing a quick screening according to the Vivifrail exercise protocol with SPPB and fear of falling. Before the intervention begins, the elderly receive an introduction to the program and during the exercise intervention, the elderly receive supervision and assistance so that the elderly can practice optimally and increase their motivation and compliance during exercise.
In the implementation of this exercise, there were no side effects that occurred in the elderly both during and after the exercise. This condition supports that Vivifrail exercises are safe to be carried out in elderly groups with pre-frailty and frailty. The results of the research and the researcher's observations while carrying out this study support that Vivifrail multicomponent exercise is so beneficial that it is recommended to be a routine exercise to be given to elderly subjects with frailty syndrome in nursing homes to improve static and dynamic balance functions. With these findings, it is hoped that further research can be carried out in a wider community and clinical setting.
Limitations in this study are as follow:
The intervention group was still given conventional exercises that are routinely given in nursing homes so that the comparison between the intervention group and the control group could not really be compared.
Conclusion
The addition of Vivifrail multicomponent training for 4 weeks in elderly people with frailty syndrome can improve statistical balance function as measured by the OLS test and dynamic balance function as measured by the TUG test.
Acknowledgements
All authors are appreciated.
Funding
None.
Authors' Contributions
All author contributed in this study.
Conflict of Interest
None.
Orcid:
Iriana Wahyu Nasifah: https://orcid.org/0009-0007-4282-5229
Damayanti Tinduh*: https://orcid.org/0000-0001-6604-8152
Indrayuni Lukitra Wardhani: https://orcid.org/0000-0002-9889-9039
Paulus Sugianto: https://orcid.org/0000-0002-0694-4075
Soenarnatalina Melaniani: https://orcid.org/0000-0002-4449-153X
--------------------------------------------------------------------------------------
How to cite this article: Iriana Wahyu Nasifah, Damayanti Tinduh*, Indrayuni Lukitra Wardhani, Paulus Sugianto, Soenarnatalina Melaniani, The effect of adding vivifrail exercises © to conventional exercises on static and dynamic balance functions in the elderly with frailty syndrome at surabaya nursing homes. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(7), 808-822. Link: https://jmpcr.samipubco.com/article_189495.html
--------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
.png)
.png)
