Document Type : Original Research Article
Authors
- Shadi Saghafi Khadem 1
- Zohre Arzaghi 2
- Behrang Rezvani Kakhki 3
- Maryam Ziyaei 4
- Fatemeh Maleki 5
- Ehsan Bolvardi 3
- Mahdi Foroughian 3
1 Department of Oral and Maxillofacial Pathology, School of Dentistry, Mashhad University of Medical Sciences, Mashhad, Iran
2 Student Research Committee, Mashhad University of Medical sciences, Mashhad, Iran
3 Department of Emergency Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
4 Department of Emergency Medicine, Faculty of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran
5 Department of Emergency Medicine, Faculty of Medicine, Birjand University of Medical Sciences, Birjand, Iran
Abstract
This study intricately explores the demographic dynamics influence on infection rates, disease severity, and mortality attributed to the virus. Through a meticulous examination of these demographic and contextual factors, we aimed at identification of high-risk individuals. Employing a cross-sectional descriptive design, this study analyzes the medical records of all patients admitted to Qaem Hospital in Mashhad, Iran, from April 2019 to September 2021 due to COVID-19. All patients who their nasopharyngeal swab tests of COVID-19 resulted positive were included in study. A Demographic data, reason for referral to hospital, length of hospitalization, and COVID-19 related death rates were collected. The findings reveal that the average age of patients was 59.22 ± 19.41 years. A notable 5.8% of the female population was pregnant. Respiratory-related complaints were the predominant reason for patient referral to hospital. Alarmingly, 28.3% of the patients succumbed to the COVID-19. The majority of patients (62%) had hospital stays of less than 5 days; 41.5% exhibited oxygen saturation levels below 90%. The majority of patients demonstrated systolic blood pressure levels between 90 and 130 mmHg. Statistical analysis showed the significant association between older age (P<0.001) and lower oxygen saturation levels (P<0.001) with increased mortality. Heightened attention should be accorded to patients of advanced age and those with diminished oxygen saturation levels. These factors emerge as valuable prognostic indicators, guiding the trajectory of each patient's disease. This early discernment paves the way for targeted health interventions, contributing to the alleviation of the mortality rate.
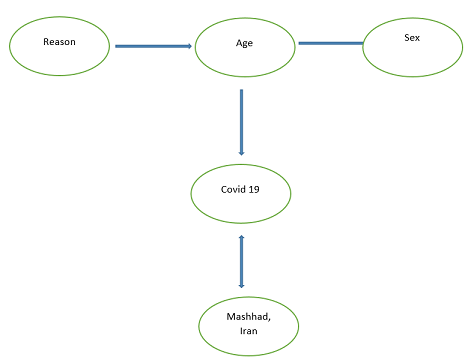
Graphical Abstract
Keywords
Main Subjects
Introduction
The proliferation of emerging and re-emerging diseases has profoundly impacted human societies, occasionally giving rise to pandemics and epidemics that precipitate global crises. At present, the paramount crisis confronting humanity is the COVID-19 pandemic, challenging even the most advanced health systems worldwide [1]. The mortality rate attributed to COVID-19 over the past year mirrors the toll incurred by the AIDS epidemic and drug overdose in recent decades [2]. COVID-19 manifests with a spectrum of severity, spanning from asymptomatic or mild cases to severe symptoms and, in some instances, fatality which was characterized by an incubation period ranging from 0 to 24 days [3]. While the disease can affect multiple systems within the human body, common symptoms encompass fever, headache, cough, fatigue, shortness of breath, sore throat, muscle pain, alterations in taste and smell, sputum production, lymphopenia, pneumonia, and hypoxemia [4,5]. A systematic review and meta-analysis of 57 studies revealed a dynamic pattern in the prevalence of COVID-19 symptoms over time, with fever prevalence ranging from 85.8% to 34.2%, cough from 83.4% to 55.3%, myalgia dropping from 53.2% to 2.5%, headache varying from 61.4% to 17.6%, and dyspnea ranging from 49.4% to 5.2%, in different general communities [6]. Hospitalization rate of COVID-19 is already variable in different settings, based on different factors [7]. Individuals with pre-existing conditions, particularly those with hypertension, and individuals experiencing lower oxygen levels may necessitate extended hospital stays [8]. The majority of patients recover through outpatient measures involving nutritional, health, and medical interventions, but approximately 14-30% necessitate hospitalization, with 2 to 6% succumbing to the disease. COVID-19 entails complications affecting cardiovascular, pulmonary, neurological, digestive, and immune systems, with underlying diseases exacerbating pathological effects on various bodily systems [9].
Several studies have provided significant data about the multifaceted nature of COVID-19, addressing aspects such as the prevalence of typical and non-typical symptoms like gastrointestinal symptoms [10], and the relationship between laboratory data profile results and the severity of pulmonary involvement in patients [11], the prognostic value of lymphocyte counts, serum CRP levels, and lung CT scan findings in predicting the final disease outcome in COVID-19 [12]. Additionally, research has been conducted to assess the prognostic value of intensive care scores in predicting 30-day mortality in individuals affected by the virus [13]. The dynamics of intensive care unit responses during different waves of outbreaks is also altered during the time [14]. Demographic factors, including age, gender, occupation, and race, wield significant influence on the incidence, severity, and mortality associated with COVID-19. This variation can be attributed to genetic disparities, physiological differences, health behaviors, access to healthcare, contact levels with patients, and immunity against pathogens [15-18]. An examination of these demographic and background factors enables the identification of high-risk individuals, facilitating early intervention strategies to mitigate mortality rates. This proactive approach is pivotal in implementing targeted health interventions and reducing the overall impact of the COVID-19 pandemic.
Methods
In this cross-sectional descriptive study, we examined the medical records of COVID-19 patients at Qaem Hospital in Mashhad, covering the period from the inception of 2019 to the September 2019. The study included individuals whose COVID-19 infection was definitively confirmed through PCR testing, in a screening program from all patients referred to hospital and hospitalized. The management of referred cases to Qaem Hospitals is contributed by collaboration among various hospital departments, including endocrinology, psychiatry, neurology, cardiology, respiratory medicine, gastroenterology, nephrology, obstetrics and gynecology, internal medicine, urology, emergency medicine, primary care/family medicine, and other specialties.
The protocol of this study was approved by the ethics in research committee of the Mashhad University of Medical Sciences. The personal information of no patient was disclosed.
The data extraction process involved documenting the patients' age, gender, and the rationale behind their hospitalization, utilizing pre-designed checklists formulated based on the pertinent information available in their medical records.
Inclusion criteria were established to include patients with a confirmed positive PCR test result, those who were hospitalized at Qaem Mashhad Hospital, and individuals whose medical records contained relevant study information. Conversely, exclusion criteria were delineated to include instances of unavailability of the patient's file, as well as the absence of pertinent study-related information in the patient's records.
Subsequent to data collection, statistical analysis was conducted employing SPSS version 26 software, employing both descriptive and inferential statistics to elucidate patterns and trends within the dataset. This methodological framework was implemented to comprehensively explore the demographic and clinical characteristics of COVID-19 patients in the specified hospital setting during the outlined timeframe.
The statistical analysis was conducted using SPSS v19, employing descriptive and analytic statistics. Descriptive statistics, including means, standard deviations, and frequency distributions, were generated to characterize the dataset. The chi-square test for independence was applied to explore associations between categorical variables. Results were considered statistically significant if p-values were below 0.05.
Results
In this comprehensive study, the medical records archive of Qaem Mashhad Hospital Government Medical Center was scrutinized, encompassing the period from the commencement of 2019 to the culmination of September 2021. Among the 14,101 individuals who sought assistance at the emergency room of Qaem Hospital during this timeframe, 7427 individuals tested positive for COVID-19 via PCR testing. The records of 4980 COVID-19-positive patients were meticulously examined, and pertinent study-related information was extracted. Regrettably, 2447 individuals were excluded from the study due to file defects. The age distribution among the patients exhibited considerable variability, ranging from under one year to 106 years. The average age of the patients was determined to be 59.22±19.41 years.
The age bracket of 61-70 years accounted for the highest number of patients, comprising 1,048 individuals (21%), while patients over 100 years old constituted the lowest number. Gender distribution revealed that out of all patients, 1,681 were female (33.8%), and 3,299 were male (66.2%), resulting in a male-to-female ratio of 1.96. Noteworthy is the identification of 99 pregnant female patients (5.8%) among those infected with COVID-19. The primary reason for patients seeking medical attention was predominantly respiratory disorders, with 39.5% of patients (1,966 individuals) presenting with such symptoms. Cold-like symptoms and general weakness followed, accounting for 9.9% (491 individuals) and 9.3% (464 individuals) of patient visits, respectively. Impaired consciousness was also identified as a significant reason for medical consultation, with 6.1% (304 individuals) of patients exhibiting this symptom (Table 1).
In this cohort of 4980 COVID-19 patients, mortality was observed in 28.3% of cases, with 1409 individuals succumbing to the disease (Table 2). Analysis of the hospitalization durations revealed that a predominant proportion, constituting 55.8% of patients, experienced a hospital stay ranging from one day to one week. Subsequently, 24.8% of patients underwent hospitalization between one week and one month (Table 2).
Among the analyzed patient cohort, the majority exhibited oxygen saturation levels below 90% (41.5%), with 37.8% falling within the 90% to 95% range and 20.7% surpassing 95% (Table 3). The mortality percentages for women and men were 27.8% and 28.6%, respectively. Statistical analysis revealed no significant correlation between gender and mortality rate (P=0.567), as presented in Table 3.
The observed mortality rate displayed an upward trajectory in tandem with advancing age, with the highest mortality rate recorded in the age group of 71-80 years old, encompassing 22.9% of the population (323 individuals). In contrast, the age group under 10 years old exhibited the lowest mortality rate, with only 0.1%, representing two individuals (Table 4). A statistically significant relationship was established between age and mortality rate, as denoted by a p-value less than 0.001 (Table 4).
Discussion
In the current investigation, the analysis revealed that the highest number of fatalities occurred in patients presenting with respiratory disorders (578 individuals), consciousness disorders (158 individuals), and general weakness (144 individuals). Notably, the mortality rate exhibited an ascending trend with decreasing oxygen saturation percentages, reaching its peak at 39% in patients with oxygen saturation below 90%. In contrast, patients with oxygen saturation percentages exceeding 95% demonstrated the lowest mortality rate, accounting for 18% of cases. A statistically significant association between oxygen saturation percentage and mortality rate was identified (P < 0.001). Examining the hospitalization duration, the highest mortality rate was observed among individuals hospitalized for one day to one week (55.6%), followed by those hospitalized for one week to one month (25.9%). Patients with hospitalization exceeding one month exhibited the lowest mortality rate at 2.4%. However, no significant relationship between mortality rate and duration of hospitalization was established (p>0.05). The overall mortality rate among patients referred to Qaem Hospital in Mashhad from April 2019 to September 2021, and subsequently hospitalized with a confirmed diagnosis of COVID-19, was 28.3%.
This finding aligns with the varying mortality rates reported in the literature. For instance, Talebi et al. reported a 13.6% mortality rate in patients with COVID-19 in Vasi Hospital in Sabzevar [19]. Mousavizadeh Jazaeri documented a 6% mortality rate in Bandar Abbas [20]. In contrast, Wang et al. noted a 4.3% mortality rate among 138 hospitalized patients [21], while Chen et al. reported a higher rate of 14.1% [22]. Additional studies by Shahriari et al. (8%) [23], Nikpour Aghdam (8.06%) [24], and Li et al. (5%) [25]. Further contribute to the observed variation in mortality rates. Such differences may be attributed to variations in sample sizes, study periods, and the temporal dynamics of vaccination efforts, which can impact mortality rates significantly.
Since the onset of the COVID-19 pandemic, age has consistently emerged as a prominent risk factor influencing morbidity and mortality. Over time, while there have been shifts in researchers' observations, the elevated risk of death have been persisted among the elderly. Reports from the Center for Disease Prevention and Control highlight a substantial percentage of COVID-19-related deaths occurring in individuals aged over 65 in the United States, underscoring the heightened risk in this demographic. Caramelo et al.'s investigation in China on risk factors for mortality due to COVID-19 confirmed age as a variable associated with an increased risk of death [26]. Similarly, Grasselli et al.'s study on risk factors related to mortality in COVID-19 patients in Italian intensive care units identified age as a significant risk factor [27]. A study conducted in England reported that over 90% of COVID-19-related deaths occurred in individuals over the age of 60, aligning with global trends in this regard. In our study, the average age was 59.22 years, comparable to findings in other studies such as Shahriari et al. (53.75 years) [23], Qian et al. (50 years) [28], and Goshayeshi et al. (67.26 years) [29]. Talebi et al. reported an average age of 57.1 years, while Chen et al. found an average age of 51 years [22]. Zhang et al.'s study of 161 COVID-19 patients reported a mean age of 45 years [2]. The convergence in average age across these studies may be attributed to the occurrence of severe symptoms and complications of COVID-19 necessitating hospitalization in these age groups, indicating the consistent impact of age as a critical determinant in the disease's severity and outcomes.
Gender has consistently emerged as a recognized risk factor in numerous studies related to COVID-19. Reports consistently indicate a higher death rate in men, with approximately 60% of deaths reported in males, aligning with the broader trends in this field highlighting an increased mortality rate in men compared to women. Some studies attribute this gender disparity to higher rates of smoking among men, leading to an elevated prevalence of underlying health conditions. In Shahriari et al.'s study, men constituted 62.8% of patients, and Nikpour reported a men-to-women ratio of 1.93 [23,24]. In our study, men comprised the majority of patients (66.2%). However, despite the gender disparity in the patient population, no significant relationship was found between gender and mortality rate. Chen et al.'s study, among 241 patients, reported a roughly equal distribution between men and women, contrasting with our findings [22]. Gender imbalances in reported cases and mortality rates may be attributed to various factors, including differences in occupational exposure, lifestyle choices, and underlying health conditions. Men, who often work outside the home, may be more exposed to the virus. Discrepancies in mortality rates may also be linked to variations in underlying health, as individuals with pre-existing conditions are more prone to severe forms of COVID-19. Notably, certain underlying diseases, such as cardiovascular conditions, are more prevalent in men. However, studies yield conflicting results on gender-related COVID-19 outcomes. While Goshayeshi et al. reported average hospitalization duration of 9 days, differing from our findings [29]. In Papizadeh et al.'s study, dyspnea emerged as the most common symptom, while Li et al. and Kim et al. noted fever, cough, and myalgia or decreased sense of smell and sputum secretion, respectively, as predominant symptoms [25, 30- 32]. Talebi et al. reported shortness of breath, cough, and fever as the most common symptoms upon arrival [19]. These variations underscore the complex interplay of demographic factors, symptomatology, and underlying health conditions in shaping the COVID-19 landscape.
Limitations, weaknesses, and strengths
Given the substantial influx of visitors to government medical centers and the constraints posed by limited medical staff, deficiencies in patient file registration occasionally arise. In addition, some patients may not furnish accurate information. Despite efforts to streamline information extraction, the electronic format of the medical citation department's archive has introduced errors or deficiencies in entering file information into the system. This electronic mode, while designed to enhance efficiency, has inadvertently contributed to challenges in maintaining data accuracy and completeness.
Conclusion
In this study, 4980 patients who visited two government hospitals in Mashhad over one year underwent examination. These substantial figures point to the disease's elevated prevalence and its capacity for rapid transmission. Of the patients examined, 2% were pregnant, signifying the vulnerability of this demographic to the disease and emphasizing the necessity for implementing essential measures and precautions to prevent infection in this high-risk population. Furthermore, old age and low oxygen saturation levels emerged as two critical factors associated with an elevated mortality rate.
Additionally, gamma-mangostin is believed to modulate cell signalling pathways that are crucial to viral replication. It may inhibit the activation of key proteins in these pathways, thus effectively impairing the virus's ability to reproduce within the host cell. This represents another avenue by which the compound exerts its antiviral effect [15,16].
An important facet of the antiviral response is the role of the immune system in recognizing and eliminating the virus. Gamma-mangostin may also enhance the host's antiviral immune response. It is thought to stimulate the production of antiviral cytokines, proteins that mediate and regulate immune responses. These cytokines can enhance the body's defence against the virus, further aiding in the control of viral infections [13-15].
Though the aforementioned mechanisms paint a promising picture of gamma-mangostin's antiviral potential, it is important to note that these mechanisms are often based on in vitro studies. The in vivo antiviral activity of gamma-mangostin, particularly its impact on viral infection and progression in a living organism, warrants further research [16,17].
In conclusion, gamma-mangostin holds promise as a potent antiviral agent, showing multifaceted mechanisms of action against various viral species. These mechanisms offer the prospect of gamma-mangostin being a broad-spectrum antiviral agent with efficacy against different viruses. However, additional studies are essential to further unravel the intricate mechanisms and validate these antiviral activities in vivo [18,19].
Efficacy against various viruses
The exploration for novel antiviral agents has led scientists to the pericarp of the mangosteen fruit, where gamma-mangostin resides. This natural compound has shown significant promise against a range of viral pathogens, offering hope for broad-spectrum antiviral applications [20-22].
Investigations into the activity of gamma-mangostin against the Influenza A virus have yielded promising results. Influenza, an acute respiratory infection, affects millions of individuals globally each year. Gamma-mangostin's ability to inhibit the entry and replication stages of this virus provides a strong basis for its consideration as a potential treatment for Influenza [23-25].
Furthermore, studies examining the activity of gamma-mangostin against the Herpes simplex virus, a widespread virus causing oral and genital lesions have reported encouraging outcomes. By preventing the virus from entering host cells and disrupting its replication process, gamma-mangostin has shown potential as a viable treatment option for managing Herpes simplex infections [22,24].
Hepatitis C, a major cause of liver disease, poses a significant health challenge globally. Research conducted on the Hepatitis C virus has shown that gamma-mangostin may interfere with the replication cycle of this virus, demonstrating potential efficacy against this disease [20-22].
In addition, gamma-mangostin's potential extends to emerging viral threats. Preliminary research suggests that it may hold potential against SARS-CoV-2, the causative agent of COVID-19. Though the studies are at a nascent stage, any potential for combating this global pandemic warrants significant interest [23,24].
Furthermore, gamma-mangostin's antiviral activity extends beyond human pathogens. Studies have indicated its efficacy against feline infectious peritonitis virus, a fatal viral disease in domestic cats. This also highlights the compound's potential in the field of veterinary medicine [25-27].
These findings suggest a broad-spectrum antiviral effect of gamma-mangostin, which is an exciting prospect. However, it is crucial to remember that much of the current research on gamma-mangostin's antiviral effects is conducted in vitro [25,26].
Translating in vitro antiviral activity to effective in vivo applications is a complex process. Factors such as bioavailability, metabolism, potential toxicity, and pharmacokinetics need to be considered, all of which require thorough investigation [27-29].
Moreover, for a better understanding of gamma-mangostin's potential as an antiviral agent, well-designed animal, and human studies are essential. The observations from such studies will help assess the real-world applicability of gamma-mangostin as an antiviral agent [30].
Gamma-mangostin, with its broad-spectrum antiviral activity, holds great promise in the fight against viral diseases. However, extensive research, including well-controlled in vivo studies and clinical trials, is needed to fully realize its potential.
Potential for future development
The journey of gamma-mangostin from the tropical forests of Southeast Asia to the realm of antiviral research is an intriguing one. Its potent antiviral activity against various viruses, as revealed by numerous in vitro studies, indeed marks gamma-mangostin as a promising candidate for future antiviral drug development [31-33].
However, the transition from in vitro success to clinical application is not without hurdles. One major challenge lies in the pharmacokinetic properties of gamma-mangostin. As a naturally occurring compound, its absorption, distribution, metabolism, and excretion in the human body require thorough investigation. Understanding these properties is vital in determining the effective dosage, route of administration, and potential side effects of gamma-mangostin as an antiviral agent [34-36].
The bioavailability of gamma-mangostin is another area that needs extensive research. The efficacy of a drug does not only depend on its ability to fight a disease-causing agent, but it also should be able to reach the target site in the body in sufficient concentration. Researchers need to determine how well gamma-mangostin is absorbed and distributed in the body to exert its antiviral effects [37-39].
The potential toxicity of gamma-mangostin, particularly at the effective antiviral concentrations, is an important aspect that needs consideration. Any adverse effects associated with its use must be carefully assessed against its potential therapeutic benefits. Rigorous preclinical toxicity studies are essential before gamma-mangostin can progress to clinical trials [40].
While current research has provided valuable insights into the antiviral activity of gamma-mangostin, there is a considerable gap in our understanding of its mechanism of action. Detailed molecular studies are required to elucidate the precise targets and pathways gamma-mangostin affects in its fight against viruses. Understanding these mechanisms will be crucial for optimizing its antiviral potential and minimizing potential side effects [41-43].
Despite these challenges, the development of gamma-mangostin as an antiviral agent is promising. Its broad-spectrum antiviral activity, combined with its potential for modulating immune responses, places it as a potential cornerstone in the treatment of viral diseases [44,45].
Efforts should be also directed towards the sustainable sourcing and production of gamma-mangostin. As a compound derived from the pericarp of the mangosteen fruit, sustainable cultivation of the plant, and efficient extraction methods should be developed to ensure a reliable supply of this potential antiviral agent [46-48].
In the face of the on-going global health challenges posed by viral diseases, the development of effective antiviral agents has never been more critical. Gamma-mangostin, with its promising antiviral properties, stands as a beacon of hope in this endeavour [49-51].
With continued research and development, and a careful consideration of the challenges ahead, gamma-mangostin could well be on its way to becoming an important tool in our antiviral armamentarium. However, as with any potential therapeutic, it is crucial that we remain guided by the principles of rigorous scientific inquiry and unwavering commitment to patient safety and efficacy [50-53].
While the road to the clinical application of gamma-mangostin is indeed challenging and long, the potential reward - a novel, effective, and broad-spectrum antiviral agent - makes this journey worth undertaking.
Conclusion
As the world grapples with the pervasive threat of viral diseases, the search for novel and effective antiviral agents remains a crucial task. Gamma-mangostin, a xanthone derivative from the pericarp of Garcinia mangostana, has emerged as a promising candidate, demonstrating in vitro antiviral efficacy against a diverse array of viruses. Despite the current gaps in understanding its detailed mechanism of action, bioavailability, and potential toxicity in vivo, the prospect of developing this natural compound into a broad-spectrum antiviral agent is intriguing and holds immense potential. However, it is crucial that this path is tread with rigorous scientific research and a patient-centric approach, ensuring both the efficacy and safety of gamma-mangostin as a future therapeutic agent. The journey ahead is challenging, but with unwavering dedication to research and innovation, gamma-mangostin could indeed illuminate a new path in the global battle against viral diseases.
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Peymanieh Educational and Research and Therapeutic Center of Jahrom University of Medical Sciences for revise manuscript.
Funding
The authors are grateful to the Research and Technology Vice-Chancellor of Mashhad University of Medical Sciences for financial support of this research.
Authors' Contributions
All authors contributed toward data analysis, drafting, and revising the article and agreed to be responsible for all the aspects of this work.
Conflict of Interest
The authors collectively grant consent for the publication of our content.
Orcid:
Shadi Saghafi Khadem: https://orcid.org/0000-0002-4910-1895
Zohre Arzaghi: https://orcid.org/0009-0008-2202-3250
Behrang Rezvani Kakhki: https://orcid.org/0000-0003-3715-6618
Maryam Ziyaei: https://orcid.org/0000-0003-1693-6818
Fatemeh Maleki: https://orcid.org/0000-0002-6823-5151
Ehsan Bolvardi: https://orcid.org/ 0000-0003-0255-1861
Mahdi Foroughin*: https://orcid.org/0000-0002-3944-9361
-----------------------------------------------------------------------------
How to cite this article: Shadi Saghafi Khadem, Zohre Arzaghi, Behrang Rezvani Kakhki, Maryam Ziyaei, Fatemeh Maleki, Ehsan Bolvardi, Mahdi Foroughian*, Demographic trends in COVID-19 prevalence at a primary hospital of Mashhad: a screening study. Journal of Medicinal and Pharmaceutical Chemistry Research 2024, 6(7), 842-854. Link: https://jmpcr.samipubco.com/article_189618.html
-----------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
.png)
