Document Type : Case Report
Authors
- Indana Lazulfa
- Neurinda Permata Kusumastuti
- Abdul Latief Azis
- Ira Dharmawati
- Arina Setyaningtyas
- Dwi Putri Lestari
Department of Child Health, Faculty of Medicine Universitas Airlangga, Dr. Soetomo General Academic Hospital, Surabaya, East Java, Indonesia
Abstract
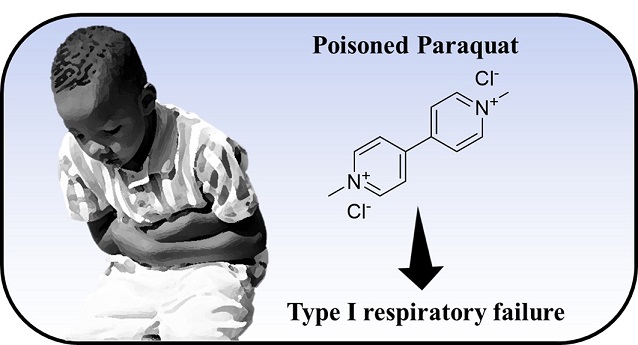
Paraquat is an organic herbicide which is widely used as a weed killer. Paraquat intoxication is lethal since there is no specific antidote. To highlight the clinical appearance and increase awareness of paraquat intoxication in children. A seven-year-old boy experienced nausea and vomiting one hour after consuming dark liquid containing paraquat. Three days later, he complained of bloody vomiting, sore throat, and abdominal discomfort and was taken to a nearby hospital. He received gastric lavage four times and was treated conservatively with intravenous fluid and H2 blockers at the High Care Unit (HCU). The patient's condition deteriorated, leading to the development of acute hepatic failure and dark urine, and then referred to our tertiary hospital for further management. Laboratory examination showed anemia, thrombocytosis, and worsening renal and liver functions. Chest x-ray revealed pneumonitis. Steroid, intravenous acetylcysteine, and hepato-protector were given. However, he died after progressive type I respiratory failure on day 14 after the ingestion. Paraquat is a common herbicide with a high mortality on ingestion since the antidote has not been found to this day. Our patient, a seven-year-old boy, accidentally ingested the paraquat. He suffered from nausea and vomiting in one hour after ingestion. Sore throat, bloody stool, vomiting, and abdominal discomfort on day 3 and yellowish skin on day 5. Even though he got further treatment, he died on day 14 after the ingestion, due to type I respiratory failure.
Graphical Abstract
Keywords
Main Subjects
Introduction
Paraquat dichloride is an organic herbicide used as a weed killer. It rapidly and effectively acts upon contact with weeds [1]. It is safe and effective when it is used according to the instructions. In some countries, paraquat dichloride is banned because of its toxicity to humans, including in the USA, but it is still used as a weed killer. Until this day, no specific antidote has been found [1,2]. When humans consume the substances, it can cause death. Symptoms sometimes appear late and if there is no information about intoxication from the family or patient, health workers may not be alerted to this situation.
In developing countries, there is a significant issue with pesticide poisoning, which is caused by the storage of dark-colored liquid in soda bottles, unmarked bottles, cups, or glasses. Paraquat was the cause of several deaths [3]. This case report is intended to highlight the clinical appearance and disease course of accidentally ingested paraquat dichloride, in a boy who is seven years old.
Case report
A seven-year-old boy came to our hospital at August 6, 2022, with the main complaint of bloody vomiting. He was referred from a local hospital with diagnoses of Gramoxone® (Paraquat-dichloride) Intoxication+hematemesis melena + Acute Kidney Injury (AKI) stage failure + Pneumonia.
Based on the interview with the family member of the patient, nine days earlier, the patient was in the rice field with his father and sipped a little amount of a dark liquid, paraquat, in a glass, and then spit it out. The patient experienced nausea and vomiting 1 hour after paraquat ingestion and was taken to primary healthcare without informing that the patient had sipped a small amount of dark liquid, he was given an anti-vomiting drug and was sent to the outpatient clinic. After three days, he reported experiencing bloody vomiting, diarrhea, sore throat, and abdominal pain and was sent to a nearby hospital. In Jombang, where he received gastric lavage four times and was treated conservatively with intravenous fluid and H2 blockers at the high care unit (HCU). The bloody vomiting and stool occurred 2-3 times per day in five days, the condition was deteriorating and the patient was referred to our hospital.
The results of the physical examination indicated head and neck area jaundice, pallor, and redness in the throat area. Abdominal examination revealed epigastric pain when pressed. Other areas were on normal examination.
Results of laboratory examination from the first hospital revealed a normal complete blood count (CBC), normal coagulation factor, normal blood glucose, and mild hyponatremia (Na 133mmol/L). On laboratory evaluation in our hospital, CBC revealed anemia and thrombocytosis (Hemoglobin levels from 12.0 to 8.0 g/dL, platelets from 491,000 to 665,000 cells/cm²), abnormal renal function (GFR 7 to 67%), worsening liver function (ALT From 149 to 341 U/L, AST From 206 to 287 U/L), hyperbilirubinemia (direct bilirubin 6.70 mg/dL, indirect bilirubin 2.50 mg/dL, total bilirubin 9.2 mg/dL), hyponatremia was corrected after 5 days admission (Na 131 to 138 mmol/L), hypokalemia (K 2.6mmol/L), and metabolic acidosis that became worsening when the patient got type 1 respiratory failure (pH 6.8, HCO3 19.1, Beecf -7.0, pO2 29, pCO2 37). Urinalysis revealed bilirubinuria and haematuria. The chest x-ray showed pneumonitis (Figure 1). The antigen test for COVID-19 was negative.
We treated this patient with nasogastric tubes (NGT) decompression and parenteral nutrition, intravenous proton pump inhibitor (PPI), intravenous tranexamic acid, sucralfate orally for gastrointestinal bleeding, and intravenous antibiotics for pneumonia. After two days, bloody vomiting and stool improved. He also got intravenous N-acetyl cysteine, ursodeoxycholic acid, and curcumin orally for cholestasis. We assessed the patient’s urine production (UP), carried out routine renal function tests, and administered serum electrolytes due to the failure stage of AKI. The UP was in normal volume with a yellowish color. The examination by the Ear, Nose, and Throat Department revealed corrosive pharynx, and no treatment was added. On day 10 after intoxication, he got worsened, fever, decrease of consciousness, desaturation, and bradycardia. We carried out Cardiopulmonary Resuscitation, but he did not respond to the CPR and died on day 14 post-injury.
Discussion
Gramoxone® (Paraquat-dichloride) is used as a strong weed-killer. Paraquat-dichloride (1,1′-dimethyl-4,4′-bipyridinium dichloride) is one of the main reasons why it is widely used as a herbicide as its ability to kill quickly through contact. This is a crystalline solid that is non-volatile and white. It can be dissolved in water, but not in most organic solvents [1,2,4].
The 2014 pesticide poisoning report in East Java, Indonesia revealed five severe cases, 120 moderate cases, and 77 mild cases. Exposure to poisoning incidents is often caused by occupational, homicidal, or accidental exposure. There are many ways in which paraquat-dichloride can enter the human body, including oral, nasal, ocular, and dermal. The lack of effective treatments and the time of therapy are the main causes of the high case fatality of paraquat-dichloride [5,6]. The estimated lethal dose in adults is 10-20 ml and 4-5 ml in children [7]. Our patient, a seven-year-old boy, sipped a dark liquid in the glass when he was in the rice field with his father. After sipping it, he spat out the liquid and his father knew that it was Gramoxone® (Paraquat-dichloride).
Our patient complained of vomiting and abdominal discomfort on the first day after ingestion. On day 4, bloody stool and vomiting, sore throat, and yellowish color in skin and urine occurred. The laboratory results indicated anemia, thrombocytosis, hyperbilirubinemia, AKI (the GFR was getting better in the laboratory assessment), and decreased liver function while the radiological examination revealed non-specific pneumonitis. After oral intake, the plasma concentration of paraquat-dichloride peaked at 2 hours, and then decreased gradually for 15-20 hours. Acute respiratory disorders, diarrhea, headache, fever, muscle pain, weakness, breathing difficulties, and nail disorder occurred after 96 hours after ingestion [5,8]. Paraquat-dichloride can cause harm to organs such as the lung, kidney, liver, muscle, and other tissues by rapidly being distributed to them after being taken orally. The lung is the primary target organ for paraquat, and it has a concentration 10 to 90 times higher than that in the plasma. The binding of paraquat to plasma protein is insufficient and renal tubules are unable to re-absorb it [7,8]. If the patients had healthy renal function, 90% of paraquat would have been absorbed into the blood and excreted through urine in 12 to 24 hours. After being absorbed by the tissue and discharged through the kidney, the remaining 10% will be released into the blood again, and the tissue could absorb the undischarged part again, creating a vicious cycle that causes continuous damage to the human body, if renal function is damaged, the clearance rate of paraquat-dichloride could decrease by 10-20%. Accidental or deliberate oral ingestion is the main cause of most paraquat-dichloride poisonings. According to the in vitro experiments, the choline transport system is involved in the transference of paraquat-dichloride through the blood-brain barrier, some symptoms of paraquat-dichloride poisoning can be reduced or prevented by the immediate administration of choline transporter inhibitors [1,3,7]. Anemia can develop when paraquat-dichloride releases iron from ferritin, leading to the conversion of ferric ions (Fe3+) into ferrous ions (Fe2+). Within the initial few days, mucosal lesions in the mouth and tongue (known as ''paraquat tongue'') develop and may become ulcerated with bleeding. The occurrence of these symptoms is not significant because they can occur even when the substance is spilt without swallowing. Our patient had corrosive pharynx, but they were not treated. Urine analysis that includes aldehydes (acetaldehyde, propanaldehyde, butanaldehyde, pentanaldehyde, hexanaldehyde, and malondialdehyde, acetone, coproporphyrin III, and 8-hydroxy-20-deoxyguanosine) can be used to determine free radical injury related to paraquat-dichloride [2]. We did not conduct examinations due to our limitation.
An initial therapy for oral paraquat poisoning is gastrointestinal decontamination using activated charcoal [10]. Our patient did not receive activated charcoal, but he received gastric lavage procedure on day 4 of the ingestion and intravenous N-acetylsistein (NAC) on day 5 of ingestion. There are no antidotes or effective treatments for paraquat-dichloride intoxications at present. This treatment targets reducing absorption and/or enhancing elimination. Therapeutic approaches should be taken before absorption when paraquat-dichloride is ingested, as it takes a while for it to be absorbed by the gastrointestinal tract. Thus, the immediate administration of activated charcoal is necessary. If gastric lavage is unavailable, it can be useful to perform it within an hour after ingestion [2,10]. Experimental animals have been shown to benefit from NAC as a hepatoprotective agent. Neutralizing free radicals and protecting cells against oxidative stress-induced damage are the benefits of NAC, a synthetic antioxidant that is derived from L-cysteine and offers protection [8]. Furthermore, our patient received tranexamic acid to stop bleeding, ursodeoxycholic acid to protect hepatocytes and cholangiocytes from intoxication-induced damage, and PPI and sucralfate to protect gastric mucous. The clinical signs deteriorated, and he died two weeks later due to metabolic acidosis and type I respiratory failure from day 13 to day 14.
Conclusion
Paraquat-dichloride is a common herbicide with a high mortality on ingestion, since the antidote has not been found to this day. Our patient, a seven-year-old boy, accidentally ingested paraquat. He suffered from nausea and vomiting in one hour after ingestion, sore throat, abdominal discomfort, bloody stool, and bloody vomiting on day 3, and yellowish skin on day 5 after the ingestion. He got gastric lavage on day 3 after ingestion, intravenous N-acetyl cysteine, PPI, sucralfate, ursodeoxycholic acid, and assessment of urine production since day 5 after ingestion in our hospital. Even though he got further treatment, he died on day 14 after ingestion due to type I respiratory failure.
Acknowledgements
We are grateful to the Dr. Soetomo General Academic Hospital, Universitas Airlangga for supporting research. Their generous funding allowed us to conduct our study and complete our work.
Funding
None.
Authors’ contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved the final manuscript for publication.
Conflict of interest
The authors declare no conflict of interests.
Orcid:
Neurinda Permata Kusumastuti*: https://orcid.org/0000-0001-7637-4285
--------------------------------------------------------------------------------------
How to cite this article: Indana Lazulfa, Neurinda Permata Kusumastuti, Abdul Latief Azis, Ira Dharmawati, Arina Setyaningsih, Dwi Putri Lestari, Deadly paraquat poisoning in a 7-years-old child: A case report. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(7), 953-958. Link: https://jmpcr.samipubco.com/article_190731.html
--------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
