Document Type : Original Research Article
Authors
Department of Radiodiagnosis, Saveetha Institute of Medical and Technical Sciences, Thandalam, TamilNadu, India
Abstract
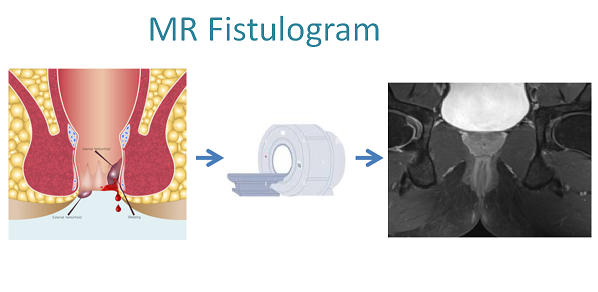
A perianal fistula, characterized by an abnormal connection between the anal canal and perineal skin, is a relatively rare yet impactful condition. Surgical management is common, but recurrence remains a challenge. Accurate preoperative assessment is crucial, and magnetic resonance imaging (MRI) plays a pivotal role in identifying tracts, abscesses, and guiding surgical decisions.The study, involved 40 patients undergoing MRI fistulography before surgical intervention. Ethical approval was obtained, and data analysis included sensitivity, specificity, positive predictive values, and negative predictive values. Imaging protocols and sequences were meticulously applied using a Philips 1.5 TESLA MRI machine.Predominantly affects males (82.5%) in the 31-45 age group, perianal fistulas were classified using MRI. The majority were Type 1 tracts (46.15%). MR demonstrated high sensitivity (89.6%) and specificity (100%) in distinguishing fistulas from sinuses and identifying abscesses (100% sensitivity and 92.3% specificity). Side branches and extensions were identified with 76% sensitivity and 100% specificity.The study of 40 cases underscored MRI's efficacy in diagnosing perianal fistulas, demonstrating 89.6% sensitivity and 100% specificity. MRI emerged as the gold standard for visualizing perianal fistulas and identifying occult sepsis, surpassing alternative imaging methods.This study concludes that MRI is a reliable preoperative tool for perianal fistulas, offering high diagnostic accuracy and aiding surgical decision-making. While proctoscopic surgery remains definitive, MRI's superiority in visualizing complex fistula tract architecture justifies its gold-standard status in perianal fistula imaging. The study highlights the MRI potential in preventing postoperative complications like anal incontinence.
Graphical Abstract
Keywords
Main Subjects
Introduction
A fistula is described as an abnormal connection between two structures, hollow viscus, or between an organ and the skin. In the context of perianal fistulas, it involves a link between the anal canal and the perineal skin [1].
Perianal fistulization is a relatively rare occurrence, with a prevalence of 0.01%, despite causing significant morbidity and discomfort. This condition predominantly affects young males, with a gender bias of 2:1[2].
The most common presenting symptoms are local pain and anal discharge [2]. Surgical intervention is typically required for fistula treatment, but it is associated with notable recurrence prevalence [3]. Accurate preoperative assessment, including understanding the primary tract's course and the presence of any secondary extensions or collections, is crucial for successful surgical management of fistulas [4].
Magnetic resonance imaging (MRI) plays a pivotal role in identifying infected tracts and abscesses that may go unnoticed in a routine proctoscopic examination [5]. Radiologists can offer detailed information about the fistulous tract and its course in relation to the external sphincter (ES) and internal sphincter (IS). This information assists clinicians in determining the most suitable surgical treatment, thereby reducing the likelihood of disease recurrence and post-surgical sequelae such as fecal incontinence [6,7].
This article aims to review the anatomy of the perianal region, the etiology, and etiopathogenesis of perianal fistula prevalence. It also provides insights into the role of imaging techniques, the protocols employed at our hospital for assessing perianal fistulas, and recent advances in MRI preoperative evaluation, including dynamic contrast sequences and diffusion-weighted imaging.
Potential novelty in the study is the inclusion of dynamic contrast sequences and diffusion-weighted imaging (DWI) in the MRI protocol for evaluating perianal fistulas. While conventional MRI sequences provide valuable anatomical information, the addition of dynamic contrast-enhanced sequences can offer insights into the vascularity and inflammation associated with fistulas. DWI, on the other hand, can aid in distinguishing between acute and chronic fistulous tracts based on the degree of diffusion restriction, thereby providing more comprehensive diagnostic information.
The objective of this study is to assess the role of MRI in the preoperative evaluation of perianal fistulas and its potential contribution to reducing the recurrence of this condition.
Materials and methods
The study was carried out at Saveetha Medical College and Hospital, following the approval from the Institutional Ethical Committee of Saveetha University. The study involved a sample size of 40 patients, selected consecutively using a specific sampling technique. The sampling process aimed to include a diverse range of patients to ensure comprehensive insights into the preoperative analysis of perianal fistulas. Informed consent was obtained prior to the study after explaining the examination procedure to the patient. Inclusion criteria include patients with perianal fistulas and patients over 18, of both genders. Exclusion criteria include patients contraindicated for MRI (e.g., patients with implants) and patients who do not consent to the study. After data collection, statistical analyses will be employed to evaluate the diagnostic accuracy of MRI fistulography, assess the correlation between preoperative findings and postoperative outcomes, and determine the overall effectiveness of magnetic resonance imaging in enhancing the management of perianal fistulas. This approach adheres to ethical guidelines and underscores the commitment to scientific rigor in the investigation of the diagnostic capabilities and advantages of MRI fistulography in the preoperative assessment of patients with perianal fistulas.
Patients included in the study underwent clinical evaluation and were referred from either the General Surgery or Surgical Gastroenterology outpatient departments of our hospital specifically for MRI fistulography. Subsequently, the fistulous tracts of the patients were diagnosed and analyzed using MRI before undergoing surgery as a therapeutic intervention. Perianal fistulous tracts are identified by high or intermediate signal intensity on T2 and T2 FS images, extending from the gluteal/perianal region to the anal canal and its surroundings. These tracts may sometimes contain debris and be associated with secondary tracts and abscesses stemming from the primary tract. Debris within the tracts manifests as small signal voids in an otherwise T2 hyperintense tract. The location of these tracts and collections varies within the perianal anatomy, often in close proximity to the anal sphincteric complex. Grading of fistulae (1 to 5) is based on their trajectory, presence or absence of collections, utilizing the St. James University Hospital classification. Active tracts exhibit restricted diffusion on DWI with corresponding ADC, especially in conjunction with abscesses, while chronic tracts do not show significant restriction on DWI. On MRI, these tracts appear as T2 hyperintense, intermediate, and hypointense on T1, reflecting the intensity of their fluid content. Given their usual presence in a background of fatty tissue (gluteal and perineal), a fat-suppressed sequence is generally preferred for assessing the tracts.
The examinations were carried out in a Philips 1.5 TESLA MRI machine. The patient was placed in the supine position in the table. The pelvic body coil was fastened around the patient’s pelvis. The following sequences are then carried out.
T2 TSE oblique axial.
DWI true axial.
T2 SPAIR OBLIQUE AXIAL/SAGITTAL/CORONAL
The parameters for the sequences are listed in Table 1.
Digital acquisition of MRI images was facilitated through a Picture Archiving and Communication System (PACS) in DICOM (Digital Imaging and Communications in Medicine) format. Radiologist-led image assessment utilized specialized software.
The evaluation of the fistulous tract involved the use of the T2 SPAIR sequence in all three planes. Sagittal and coronal planes aided in determining the height of the fistula and assessing the level of the internal opening relative to the anal verge. Axial planes were employed to examine the openings and mark their positions based on the anal clock. DWI sequences were utilized to gauge the acuity of the tract, distinguishing between chronic and acute conditions. The investigation extended to studying gluteal, ischiorectal, and pelvic collections, examining their relationships with surrounding structures. In instances of abnormalities related to extra-perineal anatomy, an additional T1 sequence was employed to detect nearby muscles.
Patients with positive MRI findings underwent corresponding surgical procedures. All surgeries, performed by general surgeons and gastroenterologists, took place under spinal anesthesia. Under spinal anesthesia and proctoscopic guidance, a probe was introduced into the external opening, attempting visualization within the anal canal. For visualized tracts, a fistulotomy was conducted. In cases where the tract was blind-ending without an internal opening, a complete fistulectomy was performed. Abscesses were typically diagnosed intraoperatively by the flow of pus through the opening upon probe manipulation or at rest.
Sensitivity, specificity, positive predictive values (PPV), negative predictive values (NPV), the range of the curve, and pain scores were computed to compare MRI findings with intraoperative observations.
Representative case
Grade V –Supralevator and Translevator Disease
Figure 1 (A, B, and C)- T2 SPAIR axial images showing a translevator abscess with extension into the pelvis resulting in left pelvic collection extending upto the left iliac fossa. It is to be noted that the anal canal is not involved in this disease. A cursory screening of the upper abdomen revealed the collection to extend into the bladder with bilateral vesicoureteric reflux.
Result
The baseline characteristics of the study participants are listed in Table 2. It was found that the majority of patients with perianal fistular disease were from the 31-45 age group in this study. A male predominance of 82.5% was noted in the study with only 7 women affected among the sample group. The most common type of perianal fistula encountered was a grade 1 with a frequency percentage of 46.15% (Figure 1).
The p-value is 0.000 (which is less than 0.005) therefore there is a statistically significant association between intraoperative and MRI findings when it comes to identifying if a tract is a fistula or a sinus (Figures 3 and 4).
The p-value is 0.000 (which is less than 0.005). Therefore, there is a statistically significant association between the MRI and Intraoperative findings (Figures 5 and 6).
The p-value is 0.000 (which is less than 0.005) therefore there is significant association of findings between MRI fistulography and proctoscopic visualization in identifying side tracts (Figure 7).
Discussion
The primary objective of this investigation was to underscore the significance of MRI fistulography in the treatment of perianal fistulas. A total of 40 cases underwent scanning, followed by surgery under proctoscopic guidance. The MRI fistulography findings were systematically tabulated, and subsequent calculations were performed to determine specificity, sensitivity, positive predictive value, and negative predictive value.
Among the 40 patients in the study group, 33 were male, constituting 82.5%, while only 7 were female. The age distribution revealed a concentration of perianal fistular disease cases between ages 31-45 (67.5%), with 8 patients (20%) above 46 and 5 patients (12.5%) below 30.
An epidemiological study by Chaparro et al.[8] encompassing 2,391 patients across 11 hospitals, supports a greater than 55% predilection of perianal fistulas in men compared to women, with a median age of 41 years. Of the 40 patients scanned, 26 had fistulas, and the remaining 14 had perianal sinuses, either simple or associated with abscess branches.
The classification of tracts revealed that 46.15% were Type 1, 19.2% were Type 2 and 3 each, and 7.6% were Type 4 and 5, respectively. MRI demonstrated a sensitivity of 89.6% (Standard error~0.049), a specificity of 100%,%(Standard error~0), and an overall accuracy of 92.5% (standard error~0.0697) to dictinguish fistulas and sinuses. For abscess identification, MRI showed a sensitivity of 100%, specificity of 92.3%, and Negative Predictive Value (NPV) of 100%.
The study identified side branches and extensions with 76% sensitivity and 100% specificity. The reduction in sensitivity may be attributed to similarities in intensity between fat and chronic small tracts lacking fluid, as well as the small caliber of the tracts compared to the main tract.
No patients in the study had associated pelvic pathology causing perianal fistulas. However, MRI's diagnostic capability extends to identifying conditions such as Crohn's disease and carcinomas. Other studies, including those by Beckingham et al. [6] and Maier et al. [9] demonstrated high sensitivity and specificity, further supporting the MRI efficacy in diagnosing perianal fistulas.
The presence of debris within the tract can cause a signal loss, potentially leading to missed tracts on MRI.This debris can obscure the visualization of the fistula tract and compromise the accurate delineation of its extent and course, leading to inadequate preoperative planning or suboptimal surgical management. To overcome these challenges, radiologists can employ strategies such as optimizing MRI sequences with fat suppression or diffusion-weighted imaging, increasing spatial resolution, utilizing dynamic contrast-enhanced techniques, acquiring multiplanar images, and correlating MRI findings with clinical data. Prospective analyses by Beets-Tan et al. [10] with a 3T MRI scanner showcased high sensitivity (100%) and specificity (86%) in diagnosing primary fistulas and their side tracts.
Though MRI is considered as the gold standard due to its superior soft tissue contrast resolution, allowing for detailed visualization of fistula tracts, associated abscesses, and surrounding anatomy without radiation exposure, MRI can be expensive and time-consuming, and it may not be readily available in all healthcare settings. Ultrasound is non-invasive, cost-effective, and widely available, making it useful for initial assessment and follow-up. It can detect superficial fistula tracts and perianal abscesses but may miss deeper or complex tracts. CT scans offer rapid imaging and can identify abscesses and evaluate for complications like fistula extension into adjacent structures. However, CT involves radiation exposure and has lower soft tissue contrast compared to MRI, limiting its ability to delineate fistula tracts accurately. In summary, while MRI is preferred for comprehensive evaluation, ultrasound and CT scans serve as valuable alternatives depending on availability, patient factors, and clinical indications.
In our setting, pre-operative MRI aided in identifying areas of occult sepsis and infection that might have been overlooked with a blind approach. In conclusion, given the convoluted nature of perianal fistulas, the intricate perianal anatomy, and the limitations of alternative imaging methods, MRI emerges as the gold standard for visualizing these fistulas. The study demonstrated high sensitivity in detecting tracts and abscesses, coupled with high specificity for tracts and branches, affirming the MRI appropriateness as a diagnostic tool for perianal fistulas and associated diseases.
Conclusion
This study underscores the MRI significance as a non-invasive and highly accurate method for diagnosing perianal fistulas before surgery. It highlights MRI's elevated diagnostic precision, sensitivity, and ability to rule out false negatives, making it a reliable tool in preoperative evaluations for this condition. Its capability to confidently diagnose primary tracts, along with their associated side tracts and abscesses amidst soft tissue and fat, is noteworthy. While proctoscopy provides definitive proof, its reliance is limited due to spatial constraints, making it challenging without the MRI assistance, which offers a superior view of the fistular tract architecture. In addition, blind proctoscopy's drawbacks include invasiveness and potential incontinence of anal sphincters, especially when performing a fistulotomy without precise knowledge of the fistula and its relationship to the anal sphincter complex. Consequently, the implementation of MRI fistulography prior to surgery proves highly reliable in identifying the presence of fistulas/sinuses with branches, abscesses, and associated pathologies, thus averting debilitating postoperative complications like anal incontinence.
Acknowledgments
The authors acknowledge the patients as a great source of learning.
Ethics declarations
Ethical Committee approval - a) Name: Saveetha institute of medical and technical science b). Registration No.: 020/05/2016/IEC/SU (B) b), date of registration: 26/05/2016, and consent to participate in the study/publication of data for research and educational purposes.
Declaration of patient consent
The authors certify that patients’ privacy was ensured and appropriate verbal and written consent was obtained.
Financial support and sponsorship
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that there are no disclosed conflicts of interest in this study.
Orcid:
Ashiq Mohammed: https://orcid.org/0000-0002-3664-4612
Ajay Lucas*: https://orcid.org/0009-0000-8522-3702
Afwaan Faizal: https://orcid.org/0009-0000-9664-6698
Paarthipan Natarajan: https://orcid.org/0000-0002-8972-5969
-----------------------------------------------------------------------------
How to cite this article: Ashiq Mohammed, Ajay Lucas*, Afwaan Faizal, Paarthipan Natarajan. The significance of Mr. fistulography in pre-operative assessments for perianal fistulas. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(7), 1010-1020. Link: https://jmpcr.samipubco.com/article_191629.html
-----------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
