Document Type : Original Research Article
Authors
1 Subspecialistic Postgraduate Program of Clinical Pathology, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
2 Department of Clinical Pathology and Laboratory Medicine, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
3 Clinical Pathology Department, Faculty of Medicine, Universitas Airlangga, Dr. Soetomo Hospital, Surabaya, Indonesia
Abstract
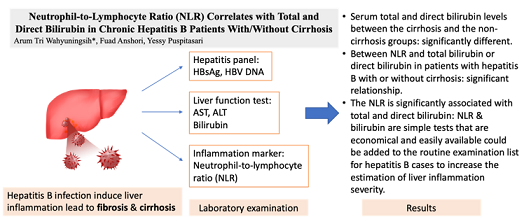
The Neutrophil-to-Lymphocyte Ratio (NLR) is considered as an important but inexpensive biomarker for inflammation in chronic hepatitis B patients. Cirrhosis increases bilirubin levels, suggesting severe liver dysfunction. This study aimed to investigate the correlation between NLR and liver function tests (LFT) in chronic hepatitis B patients with/without cirrhosis. This cross-sectional study included 36 patients with chronic hepatitis B with and without cirrhosis. The LFT results, neutrophil, and lymphocyte count were recorded and calculated. Mann-Whitney and Spearman correlation analyses were performed in both groups. A significant relationship was found between NLR and both total and direct bilirubin (r=0.35; p=0.035; and r=0.428; p=0.009). Significant differences between the two groups were found in total (p=0.01) and direct (p=0.10) bilirubin levels. The HBV-DNA was significantly positively correlated with ALT (r=0.33; p=0.047). The NLR is significantly associated with total and direct bilirubin.
Graphical Abstract
Keywords
Main Subjects
Introduction
Hepatitis B remains a persistent worldwide public health problem [1]. Hepatitis B virus patients are at high risk for progressive cirrhosis, which contributes to the disease pathogenesis of liver cirrhosis and hepatocellular carcinoma (HCC). Cirrhosis is the terminal pathway common to all chronic liver diseases [2]. Hepatitis prevalence in Indonesia has recently doubled based on 2007 Riskesdas data, increasing from 0.6% to 1.2% in 2013. In the Indonesian disease surveillance data, hepatitis B (21.8%) ranked first before hepatitis A (19.3%) and hepatitis C (2.5%) [3].
Recent studies have been conducted on inflammatory markers in the pathogenesis of liver diseases. The neutrophil-to-lymphocyte ratio (NLR) is an affordable, available, and easily quantified marker of systemic inflammation. Neutrophil counts help identify ongoing inflammation, and lymphocyte counts represent immunomodulatory pathways. Several studies have shown that NLR helps predict sequelae and mortality in patients with viral hepatitis, non-alcoholic fatty liver disease, liver transplantation, and HCC [4-8]. In developing countries with limited resources, NLR is the test of choice for prior detection of infections and inflammation.
In patients with chronic hepatitis B, hepatitis B virus deoxyribonucleic acid (HBV DNA) is regularly measured to monitor disease status and response to treatment. High levels of HBV DNA are a risk factor for fibrosis, cirrhosis, hepatocellular carcinoma, and drug resistance [9]. Liver function tests are often done to determine the integrity of liver cells in liver disease. Commonly performed liver function tests include transaminases: alanine transaminase (ALT) and aspartate transaminase (AST), in addition to total and direct bilirubin, and albumin serum levels.
Liver injury reduces the number of hepatocytes, which impairs the activity of transaminase enzymes and the process of indirect bilirubin uptake from plasma, and also reduces the transport and clearance of direct bilirubin through the bile ducts. Cirrhosis may be accompanied by a progressive increase in bilirubin. In liver failure, elevated bilirubin levels tend to spread across the blood-brain barrier. This condition can be aggravated by decreased albumin concentrations, which impede bilirubin transport [10]. Although there are many studies on NLR as a severity predictor of liver cirrhosis, as performed by Sarma [2] and Shivalingappa [11], there are still no data supporting the association between NLR and individual liver function parameters in patients with hepatitis B. This study hypothesized that NLR and the liver function tests could show the severity of liver cirrhosis even if the fibro scan test could not be performed, so it aimed to investigate the association between NLR and HBV DNA, and other liver function tests (AST, ALT, bilirubin, and albumin) in hepatitis B patients with and without cirrhosis.
Experimental
This observational analytical study involved patients with chronic hepatitis B as research subjects. Patients who were diagnosed with hepatitis B at Dr. Sardjito General Hospital, Yogyakarta, Indonesia, and had undergone testing for the HBV DNA as well as measurements of hematology laboratory parameters and liver function tests were included for this study. Individuals who had co-infections with other hepatotropic viruses and/or cardiac disorders were excluded.
Data were collected from January 2020 to November 2020. The reverse transcription-polymerase chain reaction (RT-PCR) test was conducted to measure HBV DNA levels using Cobas AmpliPrep/Cobas TaqMan (CAP-CTM) HBV (Roche Molecular Systems, Inc, CA) according to the manufacturer's instructions. The percentage of neutrophils and lymphocytes was obtained by the flow cytometry method using a hematology analyzer. Data from the liver function tests were attained using Cobas c501. Measurements of the total and direct bilirubin levels were done using the colorimetric diazotization method, while the ALT and AST enzyme activities were measured using the kinetic/enzymatic colorimetric method and albumin levels were obtained using the colorimetric assay method. Subjects were divided based on the hepatitis B severity, with or without cirrhosis.
Subjects’ characteristics data were displayed descriptively. The non-normal distribution data were displayed as median with the minimum–maximum (min-max) and the categorical data were presented in proportions with percentages (%). Mann-Whitney statistical analysis was performed to compare the characteristics of the two groups. Spearman's test was used for correlation analysis between laboratory parameters. A p-value < 0.05 was considered statistically significant.
Results and discussion
Thirty-six patients with chronic hepatitis B participated in this study with an age range of 22-76 years old and a median age of 43 years old. Male patients comprised the majority (61.1%) of the subjects, and complications of cirrhosis were observed in 13 individuals (36.1%). The median characteristics of each laboratory parameter in the subjects are presented in Table 1.
Both total and direct serum bilirubin of the cirrhosis group showed a significant increase in comparison to that of the non-cirrhosis patients, suggesting bilirubin is an important and independent risk factor for the pathogenesis of liver fibrosis. Chronic liver diseases without clinical manifestations tend to unknowingly progress into fibrosis, resulting in cirrhosis and liver failure among other severe complications. In patients with advanced cirrhosis, the impairment of glucuronic bilirubin conjugation and direct bilirubin excretion by bile led to the characteristic appearance of jaundice, making bilirubin serum concentration a potential prognostic marker in determining decompensated liver cirrhosis [10]. As pointed out by Du (2016), a positive correlation can be seen between the bilirubin concentration in all its forms and the severity of liver disease. However, bilirubin direct is noted to have a higher correlation with the liver fibrosis index [12].
There were significant differences in the values of total bilirubin (1.14 mg/dL vs. 0.35 mg/dL; p=0.001) and direct bilirubin (0.27 mg /dL vs 0.16 mg/dL; p=0.010) between the two groups (cirrhosis vs. non-cirrhosis) (Table 2). Analyses of each relationship between NLR with HBV DNA and liver function tests are presented in a scatter plot graph in Figure 1. Significant relationships were found between NLR and total bilirubin (r=0.352; p=0.035) as well as NLR and direct bilirubin (r=0.428; p=0.009). In addition, a significant relationship was found between HBV DNA and ALT (r=0.333; p=0.047), but not with AST (r=0.294; p=0.082) (data not shown). As a known precursor to liver cirrhosis, hepatic fibrosis could interfere with the normal production and excretion of bilirubin in the liver.
The NLR was significantly associated with total and direct bilirubin. Being a major marker of liver function, both total and direct bilirubin provide a relatively detailed image of changes in the liver that play a crucial role in the prognosis of acute liver disease and in monitoring chronic liver diseases. Nonetheless, anamnesis of the illness’ history, development, and other laboratory findings must always be put into consideration when deciding the final diagnosis and treatment plan [10].
The potential use of NLR levels as both an independent marker and complementary marker for prognostic and diagnostic purposes has been reported by Gong (2017) and Hussain (2020), respectively. Gong identified NLR as an independent prognostic marker for liver disease in patients with hepatitis B [5], while Hussain concluded that hyperbilirubinemia accompanied by increased NLR enhanced the accuracy of diagnostic methods to predict perforation in acute appendicitis [13]. These studies pointed out that NLR and bilirubin played a role in the detection of inflammation. Furthermore, the significant relationship shown between NLR and total bilirubin as well as direct bilirubin in hepatitis B patients were in line with our study’s findings.
The results revealed a significant relation between HBV DNA and ALT but not AST. Roushan (2005) reported similar results, showing the correlation between HBV DNA with ALT, not AST in HBeAg-negative patients [14]. As already mentioned, ALT levels above normal parameters are strongly associated with an increased risk of liver cirrhosis in those infected with HBV. Several limitations in this study include a retrospective study design that may have introduced selection bias, and the absence of some potentially helpful inflammatory markers, such as C-reactive protein (CRP) or Interleukin-6 (IL-6).
Conclusion
In comparative analyses, the serum total and direct bilirubin levels between the cirrhosis and the non-cirrhosis groups were found to be significantly different in this study. A significant relationship was found between NLR and total bilirubin and direct bilirubin in patients with hepatitis B with or without cirrhosis. In addition, a significant correlation was also found between HBV DNA and ALT. The NLR and bilirubin examination are simple tests that are economical and easily available in every laboratory and could be added to the routine examination list for hepatitis B cases to increase the estimation of liver inflammation severity. However, a further cohort study is required to observe prognostic value.
Acknowledgments
None.
Funding
This study did not receive specific grants from public, commercial, or not-for-profit funding agencies.
Authors’ contributions
ATW collected, analyzed, and interpreted the patient data and was a major contributor to writing the manuscript. FA analyzed and interpreted the patient data. YP reviewed and suggested improvements to the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
The authors declared that they have no potential conflict of interest in this study.
Orcid::
Arum Tri Wahyuningsih* : https://orcid.org/0000-0003-0131-7547
Fuad Anshori: https://orcid.org/0000-0003-0403-2264
Yessy Puspitasari: https://orcid.org/0000-0002-5790-5658
-------------------------------------------------------------------------------
How to cite this article: Arum Tri Wahyuningsih, Fuad Anshori, Yessy Puspitasari, Neutrophil-to-lymphocyte ratio (NLR) correlates with total and direct bilirubin in chronic hepatitis b patients with/without cirrhosis. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(7), 1021-1027. Link: https://jmpcr.samipubco.com/article_191631.html
-------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
