Document Type : Case Report
Authors
- Ade Ratna Ayu Vitariana 1
- Muhammad Rizki Darmawan Mustakim 1
- Muhammad Faizi 1
- Nur Rochmah 1
- Irwanto Irwanto 1
- Nining Febriyana 2
1 Department of Child Health, Faculty of Medicine Universitas Airlangga, Dr. Soetomo General Hospital, Surabaya, Indonesia, 60286
2 Department of Psychiatry, Faculty of Medicine Universitas Airlangga, Dr. Soetomo General Hospital, Surabaya, Indonesia, 60286
Abstract
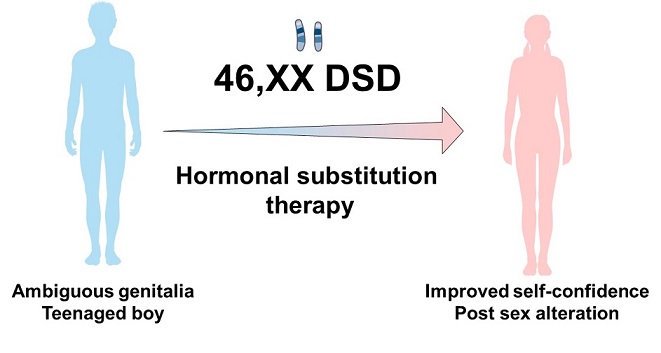
Diagnosis of ambiguous genitalia in newborns is difficult to determine, most cases in young children appear when they begin to reach puberty. We report a longitudinal case study of a child grown as a 12-year-old boy with ambiguous genitalia from a medical and psychosexual perspective. Based on the patient's medical condition, treatment adherence was excellent. This observation will continue to be monitored and assessed by educating patients to undergo monthly checkups at the pediatric endocrinology polyclinic. From the growth aspect, the patient has experienced weight loss but has not yet reached normal nutritional status. Based on the psychosexual side of the patient, there was light depression and low anxiety towards the conclusion of the patient's observation. The patient's intelligence, however, is comparable to that of children his age. After the examination, the patient was also able to adapt to life as a woman. Therefore, gender dysphoria is no longer present. In total, it was found that there was growth and development of female secondary sex characteristics in patients after consuming hormonal substitution therapy. The patient also saw an increase in the patient's self-confidence after experiencing a sex change compared to the initial observation. The patient has also legally authorized the alteration of the patient's gender.
Graphical Abstract
Keywords
Main Subjects
Introduction
The normal development of the reproductive system occurs through a phase of determination and a phase of differentiation. Disturbances that occur in one of these phases will cause the reproductive system to not fully develop, which is clinically referred to as Disorders of Sex Development (DSD). These disorders include abnormalities in the development of chromosomes, gonads, and atypical anatomy of the reproductive system [1]. An ambiguous genitalia is a form of clinical symptom that indicates the presence of DSD, although not all DSD will manifest clinically as ambiguous genitalia. This condition is a social emergency, this is related to the role of the individual in a social sphere, psychological conditions, and is related to medical complications that can occur [2].
The DSD incidence is estimated to be between 1:4500 and 1:5500 live births. Congenital adrenal hyperplasia (CAH) is the most common cause of 46,XX DSD, and estimated that 1 in 14,000-15,000 live births have CAH, but this number varies by region due to differences in the frequency of gene mutations between ethnicities. A rare cause of 46,XX DSD is aromatase deficiency (AroD). The disorder is caused by a mutation in the CYP19A1 gene that causes a decrease in the activity of the aromatase enzyme. Since its discovery in 1991, a total of only 40 AroD cases could be identified until 2019 in the world [3]. At Dr. Soetomo General Hospital, Data in 2016 showed that there were 30 patients with ambiguous genitalia who were routinely monitored at the Pediatric Endocrinology Polyclinic. This is the first case of 46,XX DSD AroD reported from this Tertiary Referral Hospital [4].
A challenge for clinicians in determining the DSD diagnosis, multidisciplinary involvement is needed in the development of diagnostic algorithms that are integrated with various technologies (including transcriptomics, epigenomics, proteomics, and metabolomics), so that the etiology of the entity can be determined. The definitive diagnosis of AroD is by analyzing the CYP19A1 gene mutation, but within the scope of limited resources, the diagnosis can be made after ruling out other causes 46,XX DSD with a detailed history, and relevant hormonal and radiological studies [3].
Comprehensive management of children with DSD requires a multidisciplinary team of experts. The main reason is that children with DSD are at risk for medical and psychosocial complications that can affect the child's quality of life. The decline in the quality of life of DSD children is mainly associated with psychosocial problems such as gender dysphoria, rejection of parents and family, feelings of shame, and social isolation [1]. Accordingly, the purpose of this long case is to report a 12-year-old child with 46,XX DSD who is considered by parents as a male since birth, so it is necessary to observe medical aspects, growth and development, psychosexual and medicolegal.
Case report
A 12-year-old with ambiguous genitalia was taken to the local hospital in July 2019 after being raised as a boy by both parents. The patient's parents finally became aware of this concern in July 2019. At that time, the patient's mother visited a urological surgeon to have a circumcision performed, but the doctor postponed the circumcision plan because the patient's testes were not palpable. Previously the patient had performed several examinations including genital ultrasonography based by a urologist. The results showed that no testes were found in either the scrotum or testicular tract in the inguinal region. Referring to an obstetrician-gynecologist, the patient underwent abdominal laparoscopy. These results showed the presence of a normal-sized uterus, both normal-sized ovaries, and a dysfunctional fallopian tube (Figure 1).
As a follow-up to the results of the examination, the patient was advised to perform a karyotyping examination. The results of chromosome analysis showed 46,XX. On other investigations, Hb levels were 14.5 g/dL, leukocytes 8910/L, Platelets 373000/L, BUN 8 mg/dL, Serum creatinine 0.4 mg/dL, potassium 3.6 mEq/L, and sodium 140 mEq/L. Based on the results of these examinations, the patient was referred to the Pediatric Endocrinology Polyclinic, Dr. Soetomo General Hospital, Surabaya in November 2019.
In the postnatal history, it was discovered that the patient was declared female at birth by the midwife who assisted with the delivery, but the midwife changed the child's sex to male the following day since the patient's urine appeared to show of a channel like a penis. The patient was born at term through normal birth at a private midwife practice on June 25, 2008. Birth weight 3400 grams, length 51 cm, cried immediately, no history of blue and yellow after birth. On genetic factors, the patient's parents did not have the same complaint as the patient. The patient is a child who is classified as intelligent even though during the pandemic the patient rarely interacts with his peers. The patient is an only child whose birth has been planned by his parents. Since childhood, both parents stated that there were no problems with the patient's development. The patient's motor skills, speech, and social relations are appropriate for children of his age.
History of growth, patients tend to have body fat since the age of 2 years. Examination of the genital organs and anthropometry are depicted in Figures 2 and 3, respectively. On examination of the genital organs (Figure 2), it was found that there was no hair around the pubic area, and the clitoris seemed elongated resembling a penis. Moreover, transverse clitoral size is 13 mm without palpable gonads. There was almost complete labioscrotal fusion with scrotal rugosity and one perineal orifice consistent with Prader stage III Genital Scale. An anthropometric examination revealed a 12-year-old girl with a weight of 59 kg (percentile 90-97), and a height of 154 cm (percentile 50-75). The ideal body weight is 45 kg. The patient's body mass index is 25 kg/m2 (90th-95th percentile) or overweight (Figure 3). Based on the medical history, physical examination, radiology, laboratory, and hormonal results showed a diagnosis of 46,XX DSD. Based on the anamnesis, physical examination, radiology, laboratory, and hormonal results, the patient was diagnosed with suspected 46,XX DSD caused by an aromatase enzyme deficiency. Based on the results of multidisciplinary discussions and patient and family decisions, the patient's parents decided to choose the female gender. Currently, the patient is undergoing hormone replacement therapy with estradiol 0.5 mg per day. The patient was also referred for psychiatric counseling at the Department of Psychiatry. He further planned reconstructive surgery after consulting with obstetrics and gynecology.
Table 1 lists a few of the patient's issues. Within a six-month observation period, the parameters of medical aspects, growth, and development, as well as levels of sadness and anxiety, will be monitored according to a predetermined evaluation schedule (Table 2). During the first month of observation, the patient was undergoing hormone replacement therapy of 0.5 mg estradiol for three months. The patient was planned for examination of the SRY gene (sex determining region of the Y) and examination of bone age. Monitoring hormone concentrations is unnecessary. In the second month, the patient reported breast soreness, particularly when touched. After using estradiol, these symptoms may be observed. The patient does not menstruate. Estradiol is still provided often and never skipped. In general, the patient's physical appearance still resembles that of a man, but the patient's hair already looks longer than before. The results of the SRY gene examination, bone age, and intelligence quotient (IQ) tests were requested by the doctor. The results of the SRY gene examination showed that no Y gene was found in the patient. This evaluation demonstrates the patient's femininity. The patient has further consulted with a child psychiatrist. Based on the results of the psychologist's observation, the patient appeared timid and closed. The results of the IQ test indicated that the patient's intelligence was average.
In the 3rd month of observation, the observer mediates with the legal aid team without the patient and family attending. The observer explained the medical condition experienced by the patient to the lawyer team to be used as a basis for making an application letter for sex change. Observation at the 4th month, the patient already looks like a woman with shoulder-length hair and wearing a headband. The patient begins to dare to communicate and looks into the examiner's eyes. At month 5, the patient was still undergoing hormone replacement therapy of 0.5 mg estradiol for three months. The patient experienced no adverse effects but felt a breast development. Menstruation has not occurred in the patient, following the doctor's plan to delay menstruation to increase the development of the patient's secondary sex characteristics. In the 6th month, the application for submitting a sex change has been administratively completed. The trial proceeded without massive impediments, and the judge approved the gender application on the same day as the trial. Evaluation of the patient's level of anxiety and depression while undergoing hormonal substitution therapy and the process of sex change, namely the Beck Anxiety Index with a value of 11 and the Beck Depression Index with a score of 21. These results indicate that the patient only experiences mild mood disorders or feelings of mild moodiness and low anxiety, including increased levels of anxiety and depression, and confidence. Patients were more emotionally and psychologically stable than in the pre-observation period.
Discussion
This case report examines abnormalities of secondary sex development in children with chromosome 46,XX (Figure 4) that have the disorder of secondary sex development. DSD is defined in the Chicago Consensus (2006) as a congenital abnormality that results in the atypical development of chromosomes, gonads, and anatomical structures of the genital organs [1,5-6].
The clinical evaluation of individuals with DSD comprises the observation of vital signs, a physical examination that includes the description of sex characteristics, and a comprehensive study of the perineal area, which contains observation, palpation, and measurement of the genital organs. The results of the genital organ examination were then modified using the Prader Scale. Accurate diagnosis also requires multidisciplinary discussion (endocrinologist, urologist, geneticist, gynecologist, pediatrician, and psychologist) [7].
The first laboratory examination included an evaluation of 17-hydroxy-progesterone (17-OHP) levels, serum electrolytes, levels of anti-mullerian hormones, and gonadotropins, accompanied by cytogenetic assessment (karyotype). In the early stages of the test, it is also required to evaluate the Müllerian Structural examination using abdomen ultrasonography [8]. Abnormalities 46,XX DSD can be caused by impaired development of ovarian structures or excess production of androgen hormones. CAH is the most common form of DSD found in karyotype 46,XX DSD because of the 21-hydroxylase deficiency (21-OHD) enzyme. Other monogenic defects in steroidogenesis can also lead to excessive androgen production. Some genetic and enzymatic deficiencies can lead to disorders of sex development (DSD) include are: enzyme deficiencies involved in the hormonal synthesis pathway leading to congenital adrenal hyperplasia, gene abnormalities involved in the development of the genital system, 21-hydroxylase deficiency which is observed in 95% of cases of congenital adrenal hyperplasia, 11 beta-hydroxylase deficiency, 3 beta-hydroxysteroid dehydrogenase deficiency, FSH receptor mutation leading to primary ovarian insufficiency, homozygous mutations responsible for 46,XX DSD with testicular or ovotesticular DSD, adrenal, renal, and pulmonary dysgenesis (SERKAL syndrome), mutation of the FSH receptor leading to hypergonadotropic ovarian failure, and other genes associated with gonadal dysgenesis in 46,XX patients, such as NR5A1, BMP15, PSMC3IP, MCM9, SOHLH1, NUP107, MRPS22, and ESR2 [9].
In the study conducted by Nasir et al. (2019), the median age of the fifteen children who had DSD was 20 months (IQR: 21 days to 7 years). Just 5/15 (33.3%) of the patients arrived during the newborn phase, while 7/15 (46.7%) of the patients were older than 2 years. Genital ambiguity was seen in ten of the fifteen patients (66.7%), while hypospadias was seen in five of the fifteen patients (33.3%). Ovotesticular DSD, which affected 60% of the research population, was the most prevalent kind of DSD in this investigation. This result is in line with South African statistics, which showed that 51% of DSD cases were ovotesticular. This is different from earlier research conducted in Nigeria as well as from most big Western series of DSD, where CAH was found to be the most prevalent DSD [10].
The results of other hormonal examinations showed an increase in the value of luteinizing hormone (LH) 27 mlU/mL (<0.1-7.8) and follicle-stimulating hormone (FSH) 50.95 mlU/mL (0.57-6.89), testosterone in the normal range of 6.89 ng/dL (3-68), and low estradiol levels <5 pg/mL (<5-20.0). Furthermore, the patient was tested for human chorionic gonadotropin (hCG) stimulation for 6 weeks and after that the laboratory results obtained testosterone 16.27 ng/dL (3-68), estradiol <5 pg/mL (<5-20.0) on day -5 and testosterone 32.27 ng/dL (3-68), estradiol <5 pg/mL (<5-20.0) on day 20. Based on the results of the hormonal examination, the patient showed an inadequate response to the hCG stimulation test. It is called an adequate response if the testosterone value is greater than the upper limit of the pubertal threshold, or the increase in the testosterone value is greater than twice the initial value [11]. Based on the results of the hCG simulation in the patient, testicular or ovotesticular abnormalities can be ruled out. The diagnosis of DSD was only made when the patient was 12 years old. Establishing DSD diagnosis in neonates is a challenge for clinicians. In many cases, genital ambiguity is evident, but the atypical manifestations of DSD in the neonate make the diagnosis difficult. The results of the assessment of the level of depression and anxiety showed that the patient experienced a mild level of depression at the end of the observation, while the evaluation of the patient anxiety level showed the result of low anxiety. The significant discrepancies between the International Statistical Classification of Diseases, Tenth Revision (ICD-10) criteria for depressive episodes and the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria for major depressive disorder (MDD) are indicated in Table 1. Initially, the DSM-5 indications for depressed mood include two symptoms of mood depression, while the ICD-10 signs include a negative view of the future. Hopelessness, which may be partially consistent with the gloomy and pessimistic perspective in the ICD-10 symptoms, was recently included in the DSM-IV to DSM-5 revision as a subjective descriptor for depressive mood. Furthermore, in the ICD-10 criteria, low self-esteem, low self-reproach, suicide, and vegetative symptoms were seen as more accurate markers of severity than other symptoms, however, in the DSM-5 criteria, all symptoms were treated equally [12,13].
Since childhood, the patient was raised as a boy, but after discussions with the patient's family, the parents decided to change the patient's gender to female. Determination of gender is essential in the management of DSD cases because this will determine further interventions in patients. This patient is medically predisposed to be female, considering the karyotype results that show chromosome 46,XX DSD. Psychosexual development is influenced by several factors, such as exposure to androgen hormones, chromosomal genes, brain structure, and social environment. The sections on Multi-Disciplinary Working, Communication, Psychological Care, Peer Group and Patient Support Advocacy, and Psychological Care are at the beginning of the new UK Guidance for the initial management of children with a suspected DSD, which was released in 2021. This recognizes that the management of children with DSD and their families is based in large part on psychosocial variables. The biological management of these diverse manifestations comes after the psychosocial sections of the guidelines. Harmonizing the psychosocial and medical priorities mentioned is challenging in practice. The task necessitates psychological input that goes beyond gender development-based education and support and instead focuses on radically improving patient-provider communication, individualizing treatment goals, and ensuring a true multi-professional approach to care planning and shared decision-making that is long-term needs-focused [14].
Kreukels et al. stated that prepubertal sex changes tend to cause gender dysphoria, and lack of self-confidence and are at risk for anxiety and depression [15]. The patient is not included in gender dysphoria, but can be at risk of experiencing gender dysphoria if the patient cannot accept the sex change conditions experienced, so psychological counseling is needed that focuses on gender identity and roles and tasks according to the gender chosen by the patient. In addition, counseling should also cover quality of life issues, a recent study showed that patients with DSD had a poor quality of life and harmed the patient's health [16]. In this case also found the presence of clitoromegaly, with normal urogenital sinus. The patient was planned for a feminization reconstructive surgery. Feminization surgery, commonly known as feminizing genitoplasty, consists of clitoroplasty, vaginoplasty, and labioplasty. These procedures can be performed separately, or together at one time [17,18]. Considerations regarding the appropriate time for feminizing genitoplasty in DSD patients are still controversial. Given that genitoplasty is frequently performed to mimic a child's genitalia, the results of this type of surgery are probably influenced by the social context of the patient. Increased stigma could have negative effects, whereas normalizing and accepting different genital anatomy could have positive effects. Parents who seek to lessen stigma by having their child's genital anatomy match their gender are in favor of early genitoplasty. While the prevalence of parents choosing not to have early genitoplasty for their child(ren) with ambiguous genitalia is unknown, certain studies indicate that most select early surgery when such procedures are offered [19].
Undoubtedly connected to parents' wishes to lessen stigma is their personal discontent with how their child's unusual genital structure appears. Parents often express discontent with their child's moderate-to-severe uncertainty after they are born with DSD. The decision for early clitoroplasty is often driven by parents and the patient's desire to have a normal appearance [19-20].
At the end of the observation period, the patient's psychosocial has improved. The patient is classified as having mild depression and low anxiety. Currently, patients are not given psychopharmaceutical drugs, but patients routinely receive psychotherapy from a psychiatrist. Successful treatment of depression and anxiety disorders in youth either psychotherapy or psychopharmacology should restore function, establish remission, and reduce the likelihood of relapse and recurrence. Due to the patient's compliance with the requirements and the backing of expert witness testimony about the patient's gender, the judge authorized the patient's request for a gender change without substantial barriers from a medicolegal perspective.
Conclusion
A longitudinal medical and psychosexual case study of a child reared as a 12-year-old boy with ambiguous genitalia has been described. Based on the patient's medical condition, excellent treatment adherence was achieved. Clinically, the patient begins to exhibit secondary female traits, particularly breast development. This observation will continue to be monitored and assessed by educating patients to undergo monthly checkups at the pediatric endocrinology polyclinic. The patient has lost weight but has not yet reached a normal nutritional condition in terms of growth. At the end of the patient's observation, based on the psychosexual aspect of the patient, there was mild depression and low anxiety. However, the patient has an average level of intelligence for his age group. After the observation, the patient has also been able to adjust to life as a woman, preventing gender dysphoria. After the study, it was determined that hormonal substitution therapy led to the growth and development of feminine secondary sex characteristics in patients. In addition, the patient's confidence was increased after undergoing a sex change, compared to the first observation. The patient has further provided legal authorization for the gender transition.
Acknowledgments
We thank to the Dr. Soetomo General Academic Hospital, Universitas Airlangga for supporting research. Their generous funding allowed us to conduct our study and complete our work.
Funding
This paper is self-funded.
Authors' Contributions
ARAV, MRDM, and NR conceptualized the methodology and software used, analyzed data, interpreted results, and wrote the initial draft of the manuscript. ARAV and NR analyzed data, interpreted results, and assisted in drafting the manuscript. II, NF, and MF critically reviewed and edited the manuscript. They also guided the manuscript writing. ARAV, MRDM, and NR collected the data, prepared the figures and tables, and analyzed the data. All authors agreed and gave final approval to the submitted manuscript.
Conflicts of Interest
The authors declare no conflicts of interest regarding the article publication.
Orcid:
Ade Ratna Ayu Vitariana: https://orcid.org/0000-0002-3443-3475
Muhammad Rizki Darmawan Mustakim: https://orcid.org/0000-0001-6041-3630
Muhammad Faizi: https://orcid.org/0000-0002-7009-4896
Nur Rochmah: https://orcid.org/0000-0002-9626-9615
Irwanto: https://orcid.org/0000-0002-7573-8793
Nining Febriyana: https://orcid.org/0000-0002-6433-5075
--------------------------------------------------------------------------
How to cite this article: Ade Ratna Ayu Vitariana, Muhammad Rizki Darmawan Mustakim, Muhammad Faizi, Nur Rochmah, Irwanto, Nining Febriyana, Medical and psychosexual aspects of a child with ambiguous genitalia: A case report. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(10), 1519-1529. Link: https://jmpcr.samipubco.com/article_195505.html
--------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
.png)
.png)
.png)
