Document Type : Review Article
Authors
- Shahram Shafa 1
- Mehrdad Malekshoar 2
- Mohammad Sadegh Sanie Jahromi 3
- Pourya Adibi 4
- Somayeh Mehrpour 5
- Lohrasb Taheri 6
- Samaneh Abiri 7
- Kaveh Hedayati Emami 8
- Tayyebeh Zarei 9
- Mansour Deylami 10
1 Department of Orthopedics, Jahrom University of Medical Sciences, Jahrom, Iran
2 Associate Professor, Department of Anesthesiology, Intensive Care fellowship, Anesthesiology, Critical Care and Pain Management Research Center, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
3 Associate Professor, Department of Anesthesiology, Jahrom University of Medical Sciences, Jahrom, Iran
4 Assistant Professor, Department of Anesthesiology, Intensive Care fellowship, Anesthesiology, Critical Care and Pain Management Research Center, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
5 Assistant professor of ICU & Critical Care Department of Anesthesiology and Critical Care, Qom university of Medical Sciences, Qom, Iran
6 Assistant Professor of Surgery, Jahrom University of Medical Sciences, Jahrom, Iran
7 Assistant professor of emergency medicine, Jahrom University of Medical Sciences, Jahrom, Iran
8 Department of Anesthesiology and Critical Care, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran
9 Assistant Professor, Department of Anesthesiology, Anesthesiology, Critical Care and Pain Management Research Center, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
10 Assistant Professor of Anesthesiology, Department of Anesthesiology and Critical Care, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran
Abstract
The review investigates challenges in implementation and presents approaches for integrating ultrasound into medical education. A thorough examination of recent literature was conducted to evaluate curriculum development for Point-of-Care Ultrasound (POCUS) education in different databases of PubMed, Web of Science, and Scopus. Qualitative thematic data synthesis was used to evaluate the collected evidence. The review identifies an increased number of studies for curriculum development for POCUS education, indicating the need for instructional adjustments. Simulation is one of the most important educational methods in this era. New teaching methods, particularly in emergency settings, enhance competency among medical residents. Studies demonstrate the value of POCUS in resource-limited environments, showing its advantages in early diagnosis and improved patient outcomes. Furthermore, assessment of POCUS skills is fundamental in its education, aligning curriculum development with learning outcomes. Emerging techniques and consensus-based checklists are advancing ultrasound skills assessment. Case studies show the positive impact of POCUS on patient care and the need for continued efforts to improve its accessibility and proficiency among medical professionals. Integrating formal training and POCUS into primary care settings are important steps for high-quality patient care, especially in the emergency room. There is a trend of increased use of POCUS education in medical universities, while standardized educational curriculums and assessment methods are still being discussed.
Graphical Abstract
Keywords
Main Subjects
Introduction
Point-of-care testing involves conducting laboratory or clinical analyses close to the patient or at their immediate location [1]. According to Precedence Research, the global market for point-of-care testing (POCT) was valued at approximately USD 32.96 billion in 2022, with projections indicating a potential surge to around USD 99.33 billion shortly [2]. Various types of point-of-care testing methods, including glucose monitoring, rapid strep tests, pregnancy tests, HIV rapid tests, influenza rapid tests, hemoglobin tests, coagulation monitoring, urinalysis strips, etc. are currently being used worldwide [1]. Point-of-care ultrasonography (POCUS) is used for immediate visualization of the human body, as a complementary tool to physical examination [3]. POCUS has different usages in medical settings, as well as high sensitivity in diagnosing various medical conditions like diverticulitis [4], skin and soft tissue abscesses [5], lung pathologies [6], etiology of shock [7], suspected intussusception in children [8], trauma assessments [9], and many more. In 1998, the first portable ultrasound prototype was created for the military [10]. Being able to skillfully and accurately conduct ultrasound exams right at the patient's bedside is crucial. According to a Delphi survey conducted among Slovenian family doctors, performing point-of-care ultrasonography in a family practice requires specialized knowledge and abilities [11]. Assessment tools like the Lung Ultrasound Objective Structured Assessment of Ultrasound Skills (LUS-OSAUS) are available to evaluate the skills of performers [12]. The acquisition of ultrasound skills is important in medical education, as shown by numerous studies. It has become increasingly integrated into curricula to adequately prepare students for clinical practice [13]. Teaching methods and potential limitations in ultrasound skills education have been investigated in other studies [14]. Simulation-based training using ultrasound simulators is one of the educational approaches [14]. The increasing importance of POCT and POCUS, along with the need for good ultrasound skills in medical education, gives a strong reason to study how we teach POCT skills.
Methods
A systematic approach was employed to identify relevant literature. Searches were conducted in reputable databases such as PubMed, Web of Science, and Scopus. Keywords and MeSH terms were utilized. Following search syntax ("ultrasound skills assessment" OR "ultrasound curriculum development" OR "POCUS education") AND ("medical education" OR "curriculum integration") AND ("point-of-care ultrasound" OR "POCUS") AND ("competency assessment" OR "skills evaluation" OR "learning outcomes") AND ("emergency medicine" OR "primary care") was used in different databases with modifications based on database. Criteria established for study selection included articles published in English, and focusing on curriculum development for POCUS education. Studies not meeting these criteria were excluded. Data extraction was performed systematically, including details on study design, population, educational settings, curriculum components, and reported challenges in ultrasound integration. A qualitative thematic data synthesis approach was employed to evaluate the collected evidence. This involved identifying common themes across the selected studies.
Methods of ultrasound skills assessment
The assessment of ultrasound skills in medical education is a dynamic field, offering diverse methods for evaluating proficiency. A systematic literature review examined the various assessment methods used to evaluate ultrasound skills in undergraduate medical education. They categorized it into objective structured clinical examinations (OSCEs), multiple choice questions, and self-assessments through questionnaires [14]. A study utilized a Delphi technique for the identification of key elements for assessing ultrasound skills, including aspects like indication for examination, equipment knowledge, image optimization, systematic examination, image interpretation, documentation, and medical decision-making [15]. However, other studies used validated assessments like Rapid Assessment of Competency in Echocardiography (RACE) or the Assessment of Competency in Thoracic Sonography (ACTS) focusing primarily on technical proficiency [12]. Another study investigated the psychometric properties of the Objective Structured Assessment Ultrasound Skill (OSAUS) scale for evaluating competence in airway assessment using ultrasound [16]. However, few studies have only focused on point-of-care ultrasonographic skills assessment. A project used a machine learning model (I3D neural networks) to automate skills assessment for Focused Assessment with Sonography in Trauma (FAST) exams, a crucial procedure for evaluating free fluid after trauma [17]. A panel of 14 POCUS specialists produced a consensus-based multispecialty checklist for evaluating fundamental POCUS skills in cardiac, lung, abdominal, vascular ultrasound, and peripheral intravenous line (PIV) insertion. With 92% of the items reaching consensus after three rounds of voting, the checklist addresses probe placement, machine setup, image quality, and anatomical identification, and includes additional criteria for PIV insertion. This makes it a comprehensive tool for assessing POCUS proficiency across a range of specialties [18]. A study employed decision tree and fuzzy rule-based methods for trainee learning assessment [19].
Curriculum development for POCUS education
In 2018, Indiana University School of Medicine initiated the development and execution of a four-year longitudinal curriculum focused on POCUS to educate medical students [20]. A proof-of-concept study was conducted to create and assess a curriculum on point-of-care ocular ultrasound designed for medical students. Medical students endorse and are in favor of a specialized educational program for POCUS [21]. The International Federation for Emergency Medicine (IFEM) Point of Care Ultrasound (POCUS) Curriculum Provides a detailed guide on creating POCUS training programs and the resources needed [22]. At Bonn University, a comprehensive ultrasound curriculum has been established for medical students during their internship year, with an emphasis on hands-on skills in ultrasound imaging. This curriculum was developed following Kern's six-step model [23]. At Harvard Medical School, a pilot curriculum for POCUS successfully was implemented along with the existing medical school program, demonstrating the feasibility of incorporating POCUS education [24].
Case studies of educational and patient outcomes of point-of-care ultrasound
Ienghong et al.'s 2022 study, conducted at Srinagarind Hospital in Thailand, focused on assessing the competency of emergency medicine residents in POCUS usage. They evaluated image acquisition, interpretation, and clinical integration. Overall image quality was rated as satisfactory (score 3.35), with OB-GYN performance being subpar. For cardiac images, acquisition skills varied from 1 to 5. Image interpretation showed 60.9% agreement, indicating a satisfactory level. Residents excelled in FAST/EFAST exams due to curriculum inclusion but struggled with OB-GYN interpretation. In terms of clinical integration, residents demonstrated good skills, with an 80.57% diagnostic accuracy rate [25].
In a retrospective study, Stolz et al. (2015) investigated the application of POCUS in a rural emergency room in Uganda, where non-physician clinicians who had completed a POCUS training program worked. The study found that POCUS was positively used in 46% of the examinations, indicating its clinical value in this setting. The results suggested that non-physician clinicians can quickly adopt and frequently use ultrasound in their practice if properly educated. However, the study encountered challenges related to machine acquisition, cost, and repair due to limited local resources and sporadic electricity. These challenges may improve as the demand for ultrasound in austere environments grows [26].
Choi et al. (2017) study introduced a structured education program for implementing POCUS-assisted physical examination in an urban tertiary teaching hospital's emergency department. The program, involving monthly sessions and chart analysis by a committee of emergency physicians, engaged 90 physicians and led to increased POCUS utilization, reduced length of stay (LOS), and a lower rate of return visits (RVs) without providing any incentives, indicating enhanced patient care efficiency [27].
Zhang et al.'s (2022) study explored the effectiveness of incorporating gamification into POCUS education as a means to enhance trainee comfort with POCUS scans in post-graduate medical education. They organized Sonowars 2020, an interdisciplinary POCUS competition and symposium, and found that this innovative approach increased trainees' comfort with POCUS scans, making it more engaging than traditional lecture or small group formats, potentially providing a solid foundation for further POCUS skill development among trainees [28].
The study by Kern et al. concentrated on how early training during medical school could increase clinician trust and utilization of POCUS in clinical settings, namely acute care settings. In 68 replies from board-certified practicing physicians in acute care specialties, they performed a poll. The results showed a significant correlation between learning POCUS early in one's medical career and higher utilization in acute settings. The findings also showed that most respondents thought POCUS improved patient outcomes and treatment, highlighting the possible advantages of early POCUS instruction during fellowship training and medical school [29].
Good et al. (2018) created a teaching tool to introduce POCUS to pediatric residents while they are doing a rotation in the pediatric intensive care unit (PICU). Focused cardiac ultrasound, lung ultrasonography, and ultrasound fundamentals were all included in the curriculum. Following their participation in the program, the residents showed a marked increase in their comfort level, awareness of POCUS indicators, and POCUS knowledge. The findings demonstrate how a foundational POCUS education could improve pediatric residents' proficiency and self-assurance in POCUS applications throughout their PICU rotation [30].
As presented in Table 1, these studies show the positive impact of POCUS on patient care and the need for continued efforts to improve its accessibility and proficiency among medical professionals. These findings provide ideas for healthcare institutions and educators aiming to integrate POCUS into their practices and training programs.
Discussion
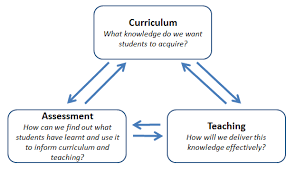
When developing curricula, it is important to determine assessment methods, particularly for practical skills like ultrasound. This approach is critical for ensuring the effective and proficient utilization of this specific technology [31]. In the methods of ultrasound skills assessment, this review showed that along with the previous checklist and instructions for ensuring excellence in ultrasound imaging, techniques such as machine learning for automation, are emerging to enhance skills assessment. The development of comprehensive, consensus-based checklists for POCUS across specialties reflects the commitment to standardizing and improving ultrasound training. As technology and expertise continue to evolve, the assessment of ultrasound skills would be a critical aspect of medical education and practice. For upcoming trials, determining the best combination of assessment methods to gauge ultrasonography skill will continue to be a difficult issue. Furthermore, it is necessary to specify standards and the frequency of student testing.
In terms of curriculum development for POCUS education our review showed in recent years, there has been a surge in curriculum development for POCUS education in medical schools [21-24]. This is in spite of the fact that not all educational programs can be readily put into practice, and numerous challenges in implementation lie ahead [20]. Moore et al. presented a methodical approach to incorporating ultrasound into the undergraduate medical curriculum of an institution facing constraints in faculty and curriculum time [32]. In a pilot study, Jujo et al. validated the feasibility of the curriculum design, highlighting the need for instructional adjustments, including modifications to the size of hands-on training groups, refining the content of cardiac POCUS lectures, enhancing hands-on teaching instructions, and optimizing the utilization of handheld ultrasound devices [33].
Finally, our review showed that structured training enhances competency among medical residents, particularly in emergency settings. POCUS proves valuable in resource-limited environments, despite challenges. In addition, innovative teaching methods and early education benefit both clinicians and patients. The findings of the Szabó et al. study showed that, when compared to traditional approaches, POCUS use helps patients with acute onset dyspnea receive a better diagnosis and experience better outcomes [34]. Much like the findings in our review highlighting the advantages of POCUS for both patients and healthcare providers, a study conducted by Carrera et al. underscores the versatile nature of POCUS. It not only enhances diagnostic capabilities but also minimizes hospital stays during emergencies, resulting in cost reductions and improved patient outcomes. However, challenges related to training and equipment costs should be tackled. Implementing formal training and integrating POCUS into primary care settings are key steps to using its benefits, and ensuring high-quality care and patient safety [35].
Based on a similar review of our study, simulation is the best education method for POCUS and is classified into two classes of static or low fidelity or advanced virtual models with high fidelity [36]. However some other authors noticed that the type of examination greatly affects the skills of performers and this factor should be considered when developing educational strategies [37]. Another important study about the national educational value of the POCUS in US showed that in different parts of the US, there are varying amounts of hours spent on lectures for POCUS, but the most important limiting barrier was financial support for educational plans of POCUS [38].
The significance of the issue was as much as in Wayne State University School of Medicine, based on the results of a pilot study, it was decided to embed ultrasound education in the training plan of first-year medical students [39]. In Germany, almost all medical universities had educational plans for POCUS in which most were using OSCE or non-standard methods of skill assessment to evaluate students' performance of POCUS [40].
Conclusion
In conclusion, assessment is a fundamental component of medical education, essential for aligning curriculum development with desired learning outcomes. The dynamic field of ultrasound skills assessment witnesses emerging innovative techniques, like machine learning for automation, alongside the development of comprehensive, consensus-based checklists to standardize and improve ultrasound training. As technology evolves, ultrasound skills assessment remains vital in medical education, although the selection of the most effective assessment method and frequency of testing pose ongoing challenges. Integrating formal training and POCUS into primary care settings are crucial steps in harnessing its benefits for high-quality patient care.
Funding
None.
Authors' contributions
All authors contributed toward data analysis, drafting, and revising the article and agreed to be responsible for all the aspects of this work.
Conflict of interest
There is no conflict of interest.
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Peymanieh Educational and Research and Therapeutic Center of Jahrom University of Medical Sciences for providing facilities to this work.
Orcid:
Shahram Shafa: https://orcid.org/0000-0001-9888-4630
Mehrdad Malekshoar: https://orcid.org/0000-0002-3361-5429
Mohammad Sadegh Sanie Jahromi: https://orcid.org/0000-0001-8437-1092
Pourya Adibi: https://orcid.org/0000-0003-2296-2166
Somayeh Mehrpour: https://orcid.org/0000-0002-2626-5272
Lohrasb Taheri: https://orcid.org/0000-0002-3702-2778
Samaneh Abiri: https://orcid.org/0000-0002-0224-5672
Kaveh Hedayati Emami: https://orcid.org/0000-0001-5920-396X
Tayyebeh Zarei: https://orcid.org/0000-0001-8605-7742
Mansour Deylami: https://orcid.org/0000-0002-5933-3219
---------------------------------------------------------------------------------------
How to cite this article: Shahram Shafa, Mehrdad Malekshoar, Mohammad Sadegh Sanie Jahromi, Pourya Adibi, Somayeh Mehrpour, Lohrasb Taheri, Samaneh Abiri, Kaveh Hedayati Emami, Tayyebeh Zarei, Mansour Deylami*. Ultrasound skills assessment and curriculum development in medical education: a narrative review, Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(1), 72-81. Link: http://jmpcr.samipubco.com/article_182801.html
---------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
