Document Type : Original Research Article
Authors
- Arman Hakemi 1
- Sahar Nosrati 2
- Seyed Reza Habibzadeh 3
- Majid Khadem Rezaiyan 4
- Maryam Ziyaei 5
- Roohie Farzaneh 3
- Fatemeh Maleki 6
- Mahdi Foroughian 3
1 Department of Emergency Medicine, Shahroud University of Medical Sciences, Shahroud, Iran
2 Student Research Committee, Mashhad University of Medical Sciences, Mashhad, Iran
3 Department of Emergency Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
4 Department of Community Medicine, Factuly of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
5 Department of Emergency Medicine, Zahedan University of Medical Sciences, Zahedan, Iran
6 Department of Emergency Medicine, Faculty of Medicine, Birjand University of Medical Sciences, Birjand, Iran
Abstract
This study aimed to determine and compare the negative pressure in tracheal and esophageal intubation in the corpses immediately after the end of cardiopulmonary resuscitation. The current cross-sectional study was conducted in the emergency departments of Imam Reza and Ghaem hospitals in Mashahd, Iran, in 2021 and 2022. The target population consisted of patients who had undergone unsuccessful cardiopulmonary resuscitation and had died. After obtaining consent from the families of the patients who died in the emergency department. We included their bodies in the study immediately at the end of the unsuccessful cardiopulmonary resuscitation. Exclusion criteria included confirmed oesophageal disease or musculoskeletal disorders. To record the pressures, we simultaneously placed the tracheal tube in the oesophagus and trachea, and the negative pressure inside them was measured by a manometer connected to the suction device, and then the pressure inside the oesophagus and trachea of the corpses was recorded. A total of 30 corpses were examined, among which 20 were male (66.7%) and 10 (33.3%) were female. Their mean age was equal to 49.86 ± 19.97 years with the range of 23 to 78 years. The average negative pressure of the oesophagus was 494.00 ± 13.66, and the average negative pressure of the trachea was 319.60 ± 14.59. The maximum and the minimum negative pressures of the oesophagus were 479 and 553, respectively, and those of the trachea were 290 and 343. There was a significant difference in terms of negative pressure between the oesophagus and trachea (p<0.001). In general, the negative pressure of the oesophagus was significantly higher than that of the lungs. This can be used in future studies to attain a correct diagnostic method to differentiate correct endotracheal intubation from oesophageal intubation.
Graphical Abstract
Keywords
Main Subjects
Introduction
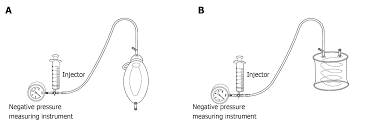
The act of achieving a safe passage for the air through the use of endotracheal intubation is a crucial expertise in the fields of emergency medicine and anaesthesia. An incorrect positioning of the tube in the esophagus is a notable contributor to the occurrence of disability and mortality [1]. Studies have revealed that about 2.9-16.7% of endeavours to perform emergency endotracheal intubation result in the positioning of the tracheal tube within the oesophagus [2]. There exist several conventional techniques employed to verify the accurate positioning of the endotracheal tube. Such techniques include directly observing the vocal cords, assessing the chest expansion, and conducting chest auscultation. Although auscultation is typically considered as the primary method of confirmation, an additional method of confirmation such as quantitative waveform capnography or observation of ventilator waves is also routinely utilized. It is important to note, however, that each the mentioned method possesses its own limitations and may not consistently provide an identical and dependable answer in patients with physiological variations [3]. One of the factors that have long been taken into account when distinguishing between the positioning of the tracheal tube in trachea and oesophagus is the disparity in pressure within the oesophagus and trachea. The wall of the oesophagus typically remains flat, whereas the trachea is kept open by C-shaped cartilages. Hence, in theory, the pressure within the esophagus is expected to be higher than that within the trachea [4]. Kasper et al. also replicated their investigation in the year 1998 within the restrictions of the United States. In a cohort of 300 patients who underwent intubation, the attachment of an ambu bag to the terminus of the tracheal tube served to confirm the placement of the mentioned tube. Following the evacuation of the air from within the bag, a period of ten seconds was allowed to elapse, during which the re-expansion of the bag was observed. The confirmation of endotracheal tube placement was validated if the ambu bag returned to its initial state within this predefined time frame. The results of their investigation demonstrated that this method revealed a sensitivity of 100% in ascertaining the correct position of the tracheal tube within the oesophagus [5]. Despite the considerable sensitivity shown by these methods, which were devised in accordance with the inherent disparity in pressure between the trachea and oesophagus, their principal drawback lies in their protracted nature during critical junctures of the patient rescue. Given the aforementioned challenges, such investigations have subsequently ceased to be pursued and are effectively excluded from clinical applications [6]. Our study indicates that by quantitative determination of the disparity in negative pressure between the oesophagus and trachea, rather than relying solely on theoretical and qualitative means, it may be feasible to employ a barometer connected to the suction apparatus to measure this negative pressure. The use of this method allows for prompt removal of the endotracheal tube. In theory, this approach has proved to be more effective than all the previously devised approaches that rely on the pressure difference between the oesophagus and stomach. Moreover, within a short time, it enables differentiation between the placement of tracheal tube in either the oesophagus or trachea. The use of this technique in patients during intubation necessitates, initially, the assessment of the suction level in the trachea and oesophagus of various patients in the state of respiratory arrest. Any delay, even if only a few seconds, in the execution of the procedure outlined in this investigation results in a delay in rescuing the patient and contravenes ethical principles [7]. The incorrect placement of the endotracheal tube in the oesophagus has been identified as a significant contributing factor to disability and death. It is worth noting that the pressure levels within the oesophagus are higher compared to the trachea. Although there are methods developed to address this issue, they tend to be time-consuming and are not commonly utilized at the patient's bedside. In this study, a manometer connected to a suction device was used to quantitatively measure and compare the negative pressure within the oesophagus and trachea. We hypothesized that by measuring this negative pressure difference with a barometer connected to the suction device, it would be possible to determine the tracheal tube positioning within a short period.
Material and methods
The current descriptive cross-sectional study was conducted in the emergency departments of Imam Reza and Ghaem hospitals in Mashhad, Iran, in 2021 and 2022. After the project was approved by the research vice-chancellor of Mashhad University of Medical Sciences and the university Ethics Committee with the code no. IR.MUMS.MEDICAL.REC.1400.342, the study was started. Given the alpha error of 5% and d=0.18, the sample size was estimated 29 subjects, which was increased to 33 in each group by considering 10% attrition. The target population consisted of patients who had undergone unsuccessful cardiopulmonary resuscitation and unfortunately had died. Cardio-pulmonary resuscitation was terminated after long efforts and with the doctor discretion, while considering the principles of medical and professional ethics. In case the families of the patients who died in the emergency department of Imam Reza and Ghaem hospitals in Mashhad gave their consent, their bodies were included in the study immediately after the unsuccessful cardiopulmonary resuscitation. Exclusion criteria included known oesophageal disease or musculoskeletal disorders. The negative pressure inside the oesophagus and trachea was measured by a manometer connected to the suction device, and then the pressure inside the oesophagus and trachea of the corpses was recorded. SPSS version 26 was used to analyse the data. To check the qualitative data, we used the Chi-Square test and the frequency and percentage of the data. Also, to examine the quantitative data, we used central and dispersion indices including mean, median, standard deviation, and interquartile range. To compare the qualitative data related to the pressures between the oesophagus and trachea, we initially checked the normality of the data using the Kolmogorov–Smirnov test, and if normal, the independent t-test was used. Otherwise, the Mann-Whitney test was used. P-values less than 0.05 were considered significant.
Results
A total of 30 corpses were examined, among which 20 were male (66.7%) and 10 (33.3%) were female. Their mean age was 49.86 ± 19.97 years (Table 1).
Table 2 also presents the average, standard deviation, and the maximum, and minimum negative pressure of the esophagus and trachea among the studied cases. The average negative pressure of the oesophagus was 494.00±13.66 and the average negative pressure of the trachea was 319.60±14.59.
Table 3 compares the average negative pressure between the oesophagus and trachea. Comparison of the mean negative pressure between the oesophagus and trachea was significant (P<0.001).
Discussion
In general, our findings demonstrated a notable disparity in the negative pressure of the trachea and oesophagus. Specifically, the negative pressure within the oesophagus was significantly greater than that observed in the trachea. Based on these recorded values, it is plausible to employ this approach in distinguish between accurate and inaccurate intubation through conducting further studies and considering the average pressure of both organs. Nevertheless, further investigations in this field are required. Numerous studies have been carried out to distinguish between tracheal and oesophageal intubation, exploring various methods to avoid incorrect intubation. Although several techniques exist for assessing and distinguishing improper esophageal intubation, it is worth noting that no previous study has examined the method employed in the present investigation for differentiation. Chen et al. [8] employed ultrasound in a study conducted in 2020 to discern between oesophageal and pulmonary intubation. The examination was carried out on a cohort of 118 patients who had undergone emergency intubation within the specialized care unit. A study was carried out to compare the diagnostic efficacy of ultrasound with fiberoptic bronchoscopy. The sensitivity, specificity, positive predictive value, and negative predictive value of ultrasound were determined to be 75%, 100%, 100%, and 97.2%, respectively. Furthermore, a Kappa value of 0.844 was documented. In summary, this study concluded that ultrasound had a substantial diagnostic value in the identification of incorrect oesophageal intubation. Chowdhury et al. [9] conducted a separate research in 2020 to compare the efficacy of ultrasound with alternative techniques in diagnosing endotracheal intubation. The researchers in this study examined 120 patients, with a first-year resident administering Internet anaesthesia. The findings indicated that ultrasound was the most rapid method in identifying accurate intubation, surpassing the effectiveness of solely relying on the lung sound from one side, lung sound from the two sides, the first wave of capnography, and the sixth wave of capnography. The overarching conclusion drawn from this study suggests that when a patient is being prepared to be anesthetized, ultrasound serves as the optimal approach to ensure pulmonary intubation is carried out correctly. Patil et al. [10] carried out a further investigation in 2019 on the diagnostic value of ultrasound in distinguishing between endotracheal intubation and endoesophageal intubation. Their research was conducted on a total of 89 patients who were admitted to the intensive care unit and required pulmonary intubation. The occurrence of endoesophageal intubation in this study was found to be 2%. The results of their study revealed that ultrasound exhibited a sensitivity of 96%, specificity of 100%, and an accuracy of 96% when distinguishing between oesophageal and pulmonary intubation. Hansel et al. [11] in a systematic review study in 2023 compared different methods of differentiating the esophageal from pulmonary intubation. Their investigations were done on 4 cases, which included misting, lung auscultation, 5-point auscultation, and oesophageal detector device. The sensitivity of misting, lung auscultation, 5-point auscultation, and oesophageal detector device was reported as 98%, 89%, 94%, and 96%, respectively. In addition, the false positive rate in lung auscultation, 5-point auscultation, and oesophageal detector device methods was reported 69%, 14%, 18%, and 5%, respectively. As indicated in the aforementioned studies, there exist various approaches in distinguishing between pulmonary and esophageal intubation. Capnography has been identified as one of the most precise methods. However, its accessibility is limited to certain areas [9, 12]. Another method involves the utilization of ultrasound, yet its availability is not universal, and the developing nations encounter obstacles in implementing these two methods [9]. It should be noted that the applying pulmonary auscultation as a means of differentiation may at times lack accuracy due to the patient's specific condition [13].
Limitations, weaknesses, and strengths
The present study was subject to some limitations. The sample size utilized in this study is one of its limitations. Another shortcoming is the absence of a universally recognized reference technique for discerning between the pulmonary and oesophageal intubation, as well as comparing the negative pressure method with the afore-mentioned technique. Nonetheless, our study represents the inaugural inquiry of its nature, rendering it of considerable significance and constituting a favourable aspect in and of itself.
Conclusion
In general, the results we obtained demonstrated a notable disparity between the negative pressure levels in the oesophagus and trachea, with the former being considerably higher. This distinction bears significance as it can potentially help to identify and distinguish between correct pulmonary or oesophageal intubation. Notwithstanding, further investigations are warranted to establish a comprehensive understanding of these findings. It is suggested that it should be noted that the existing techniques either lack the necessary sensitivity or are severely limited in their applicability. The development of a novel approach, therefore, holds promise in terms of life-saving potential for patients.
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Ghaem Educational and Research and Therapeutic Centre of Mashhad University of Medical Sciences for providing facilities to this work.
Suggestions
It is suggested that further studies should be conducted with a larger sample size while considering the diagnostic gold standard methods so that negative pressure can be used to differentiate between the two types of intubations.
Ethical considerations
A written informed consent was obtained from the relatives of the deceased to participate in the investigation. The patients’ data were encoded and documented with the exclusion of any identifying information to uphold confidentiality. This study adhered to the ethical principles of Helsinki. Furthermore, the Ethics Committee of Mashhad University of Medical Sciences approved all stages of the study.
Funding
The authors are grateful to the Research and Technology Vice-Chancellor of Mashhad University of Medical Sciences for financial support of this research.
Conflict of interest
There is no conflict of interest.
Authors' contributions
All authors contributed toward data analysis, drafting, and revising the article and agreed to be responsible for all the aspects of this work.
Orcid:
Arman Hakemi: https://orcid.org/0000-0002-9779-047X
Sahar Nosrati: https://orcid.org/ 0009-0003-2873-5367
Seyed Reza Habibzadeh: https://orcid.org/0000-0003-4569-1776
Majid Khadem Rezaiyan: https://orcid.org/0000-0003-2698-176X
Maryam Ziyaei: https://orcid.org/0000-0003-1693-6818
Roohie Farzaneh: https://orcid.org/0000-0002-0892-1555
Fatemeh Maleki: https://orcid.org/0000-0002-6823-5151
Mahdi Foroughian: https://orcid.org/0000-0002-3944-9361
-------------------------------------------------------------------------------------------
How to cite this article: Arman Hakemi, Sahar Nosrati, Seyed Reza Habibzadeh, Majid Khadem Rezaiyan, Maryam Ziyaei, Roohie Farzaneh*, Fatemeh Maleki, Mahdi Foroughian, Investigating the difference of negative pressure in tracheal and esophageal intubation immediately after the end of cardiopulmonary resuscitation in patients referred to the emergency room. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(1), 82-88. Link: http://jmpcr.samipubco.com/article_182804.html
-------------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
