Document Type : Short Communication
Authors
Department of Pediatrics, Faculty of Medicine Universitas Airlangga, Dr. Soetomo General Academic Hospital, Surabaya, East Java, Indonesia
Abstract
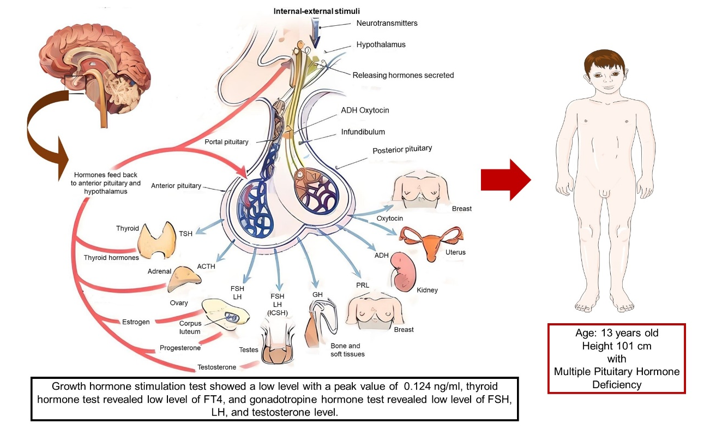
Multiple pituitary hormone deficiency (MPHD) is a disorder that can cause short stature and delayed puberty due to the deficiency of several pituitary hormones. This case report aimed to deliver a rare case of multiple pituitary hormone deficiencies, focusing on the diagnosis approach and therapy. A thirteen-years-old boy came with a main complaint of short stature with a height of only 101 cm. The growth chart showed that the patient was below the third percentile. The Tanner stage was prepubertal. There was no history of short stature, delayed puberty, and hormonal disorders in his family. Hormonal tests showed deficiencies of GH, FT4, FSH, LH, and testosterone, and normal serum levels of TSH. Those were indicating growth hormone deficiency, central hypothyroidism, and hypogonadotropic hypogonadism. Patients received levothyroxine and recombinant human growth hormone as hormone replacement therapy based on the etiology. The evaluation of therapy is carried out every 3-6 months. MPHD may be idiopathic or caused by hereditary disorders. The underlying cause of MPHD remains unknown. Further screening and diagnosis are required to evaluate risk factors and the best future therapy.
Graphical Abstract
Keywords
Introduction
Multiple Pituitary Hormone Deficiency (MPHD) is an endocrine disorder caused by a deficiency of more than one pituitary hormone [1]. It may be caused by acquired hypothalamic-pituitary abnormalities such as a tumour, surgery, trauma, or irradiation. They can also be idiopathic or the result of hereditary disorders. In 10% of cases, congenital MPHD is familial; however, it is frequently sporadic [2]. MPHD is a known cause of short stature and delayed puberty in children.
Short stature itself is one of the most common reason children are taken to a pediatrician, either because of the wishes of the parents or a referral from a family doctor. The main aim of evaluating short stature in children is to identify a number of children with pathological causes, whether non-endocrine or endocrine causes. The cause of endocrine disorders is a small percentage, but it is important because if diagnosed it can be treated. Considering that there are so many differential diagnoses for short stature, an appropriate history and physical examination is needed to determine which supporting examination to choose, and to distinguish pathological forms from normal variants. Therefore, it is very important to evaluate carefully when facing patient with short stature. The objective of this case report is to present a rare case of a child with short stature due to multiple pituitary hormone deficiency, focusing on diagnostic approach and therapy.
The MPHD can be observed in a short stature child, which is due to Growth Hormone (GH) deficiency as well as other pituitary hormone deficiency, especially thyroid hormone (TSH) [3]. The pituitary also produced Follicle-stimulating hormone (FSH) and Luteinizing hormone (LH). Therefore, deficiency in any of those hormones can cause an absence of signs of sexual maturation. The condition is called delayed puberty [4].
The prevalence of MPHD is estimated to be 1 in 8000 individuals worldwide [5] while congenital MPHD has an incidence of 2 in 100,000 live births [6]. Research conducted on 115,000 children in the United States reported that of 555 children with a growth rate of less than 5 cm in 1 year, only 5% had endocrine disorders while the other 95% did not have endocrine disorders. Research conducted in Iran showed that the percentage of short stature that was caused by Growth Hormone Deficiency (GHD) was 6.1% [3] while delayed puberty itself occurs in 5% of the population.
MPHD, which causes short stature and delayed puberty, can create various social issues. A study of children with growth retardation have shown severe deficits in emotional development, including a lack of aggressive drive and abnormal object relationships. Children with short stature also showed shyness, impaired self-concept, and social withdrawal [7].
Patients with pituitary hormone deficiencies must be aware of other pituitary hormone abnormalities. It appears to be a dynamic condition in which new deficiencies might arise years after the initial diagnosis, and all hypopituitary patients should have regular endocrine follow-ups. This case aimed to deliver a rare case of multiple pituitary hormone deficiencies, focusing on diagnosis approach and therapy.
Case Report
Informed consent was obtained from the patient's mother. A 13 years old boy came to the Pediatric Endocrinology outpatient clinic with a chief complaint of short. He looked shorter than his peers since he was five years old. He was 101 cm in the first admission (Figure 1). When he was six years old, he was only 89 centimetres (cm) tall, and when he was 11 years old, he was 98 cm tall. He had not yet experienced wet dreams or any changes in his voice. No hair had grown either on his face or body.
He was said to eat properly and drink milk on a daily basis. He never complained of recurrent vomiting and/or diarrhea. He never complained of severe or prolonged headache. He also never complained of any visual impairment. There were no history of consuming prolonged medication or experiencing chronic diseases. There were no previous history of radiation, chemotherapy, or organ transplantation. There was no previous history of a head injury. He had completed all childhood immunization. His developmental milestone was within normal limits. He also had a good school performance.
He was born prematurely by caesarean section at 34 weeks of gestation due to premature rupture of membranes. His birth weight was 1750 grams and his height was 48cm. Based on Lubchenco's score, he belonged to appropriate for gestational age. He was the second child in his family. His sibling was a 17 years old girl with normal weight and height.
There was no history of short stature, delayed puberty, and hormonal defects in his family. His mother had menstruation at the age of 12 years and his father experienced wet dreams at the age of 13 years.
The patient had a weight of 14 kg, a height of 101 cm, and a head circumference of 48.5 cm. Patients with an ideal body weight of 16 kg, and the percentage of ideal body weight was 87.5% indicating moderate malnutrition. Based on Centre for Disease Control (CDC) growth chart, his height was under the third percentile (Figure 2). Based on the Nellhaus chart, the head circumference was microcephaly. His father's height was 160 cm and his mother's height was 145 cm. His mid-parental height was 159 cm and his genetic potential height was 145.5 cm to 162.5 cm.
Physical examination showed that both testicles were palpable with volume 2 ml each. The upper per lower segment was proportionate with the ratio of 1.25 (upper segment was 56.3 cm and lower segment was 44.7 cm). His face and body did not show characteristics of dysmorphic features. There had not been any hair growth on his face, his armpit, and his genitals. There was no breast enlargement. Tanner's stage was prepubertal (G1P1A1).
From the history taking and physical examination, this patient assessment indicates short stature and delayed puberty. To determine the etiology, we performed bone age test, growth hormone stimulation test, and also thyroid and gonadotropine hormone test.
The first simple imaging examination was bone age (Figure 3). The bone age result was 2 years and 8 months. It meant that this patient had delayed bone age. These data distinguished this patient from those with familial short stature, in whom bone age corresponds approximately to chronological age. This patient with a chief complaint of proportionate short stature, delayed puberty, no dysmorphic feature, and had delayed bone age. This condition could be due to an endocrine disorder. Therefore, we performed some hormonal examinations to look for any hormonal defect.
First, we identify if there is a growth hormone deficiency, as growth hormone plays a role in all phases of growth, both prenatal and postnatal [3]. We performed a growth hormone stimulation test using Clonidine. Before starting the test, the patient was fasting for 8 hours. Baseline growth hormone level was taken at minute 0 and the result was 0.05 ng/mL, and then Clonidine 5 mcg/kg BW was given orally. Growth hormone level was 0.05 ng/mL, 0.124 ng/mL, 0.05 ng/mL, and 0.05 ng/mL at minute 30, 60, 90, and 120, respectively. We could conclude that the growth hormone stimulation test revealed a low level of growth hormone with a peak value of 0.124 ng/mL (normal level > 7ng/mL). This was indicating growth hormone deficiency. We also measured thyroid hormone to identify hypothyroidism, as thyroid hormone deficiency can cause growth retardation and cessation of bone maturation [3]. The Free T4 (FT4) level was 0.65 ng/dl (normal range 0.8 to 1.9 ng/dl), and the TSH level was 2.87 uIU/ml (normal range 0.4 to 4.2 uIU/ml). This was indicating central hypothyroidism. Then we measured gonadotropine hormones, as it is important in the process of stimulating growth and inducing secondary sexual growth [3]. Gonadotropine hormones were also low; the LH level was 0.5 mIu/mL (normal range 1 to 1.25 mIu/mL), the FSH level was 1.41 mIu/mL (normal range 1.5 to 11.8 mIu/mL), and the testosterone level was 0.09 ng/mL (normal range 2.2 to 10.5 ng/mL). Those data were indicating hypogonadotropic hypogonadism that was the cause of delayed puberty. From the history taking, physical examination, bone age, and hormonal examination, we assessed this patient with short stature due to growth hormone deficiency and central hypothyroidism, and also delayed puberty due to hypogonadotropic hypogonadism. This condition was called multiple pituitary hormone deficiency (MPHD) (Figure 4). To identify the etiology of MPHD and to ensure there was no intracranial mass, we performed a head MRI. Fortunately, the head MRI revealed normal. This patient with MPHD displayed a short stature and delayed puberty. The patient got hormone replacement therapy with recombinant human growth hormone subcutaneous injection that was taken once a day at night with a dosage of 25 mcg/kg/day (0.3 mg per 24 hours) and levothyroxine that was taken once a day with a dosage of (~100 mg/m2). Evaluation of therapy is carried out every 3-6 months. The height was increase 2.5 cm during the first 3 months of treatment.
Discussion
This patient came with a chief complaint of being shorter than his peers. The first thing to do when facing patient with short stature is to take measurements of height accurately and then do a proper plot based on the appropriate growth curve. For a 13-year-old kid, this patient was only 101 cm tall. When we plotted on the CDC growth chart, his height was under the third percentile. Short stature is a term for height under the third percentile or - 2 SD according to age and sex on the growth chart which is used in the population [3].
There are so many etiologies for short stature (Figure 5), therefore proper history taking and physical examination are needed. Therefore, we have to do a thorough examinations to exclude the differential diagnosis. Short stature is divided into two classification, which are non-pathological short stature (normal variant) and pathological short stature. Non-pathological short stature is further divided into familial short stature and constitutional delay of growth and puberty (CDGP) [3,9].
Familial short stature is caused by genetic factors. It is almost always accompanied by short stature on one or both of the parents. All the laboratories examination in familial short stature is normal, bone age is normal, and there is no endocrine abnormality [3]. This patient did not belong to familial short stature because he had abnormal bone age and hormonal level, and his parents was not short stature.
The second type of nonpathological short stature is a constitutional delay of growth and puberty (CDGP), which has characteristics of delayed linear growth in the first three years of life which is followed by normal growth. In this type of short stature, there was no abnormality of endocrine function [3]. In this case, the patient did not belong to CDGP because he had an endocrine abnormality.
This patient did not belong to both kind of nonpathological short stature, which is familial short stature and constitutional delay of growth and puberty (CDGP). Therefore, the next step was to look for the etiology of short stature from the pathological one. Pathological short stature is subdivided into proportionate and disproportionate short stature [9]. This patient with normal upper per lower body ratio belonged to the proportionate short stature. Pathological proportionate short stature is further subdivided based on whether this patient has a dysmorphic feature or not [9]. This patient had no dysmorphic feature so we could exclude the possibility of syndromic disease in this patient.
Thereafter, we should further identify the etiology of pathological proportionate short stature in this patient. From history taking, we could exclude the etiology of deprivation, medicine, and chronic disease. Therefore, the most possible etiology was due to endocrine disorder [9]. In fact, after the growth hormone stimulation test and also thyroid and gonadotropine hormone test were done, all the results were abnormal, showing an endorine disorder.
Growth hormone stimulation test revealed a low level of growth hormone with a peak value of 0.124 ng/ml (normal level>7 ng/ml). It was indicating a growth hormone deficiency. Growth hormone is a polypeptide hormone secreted by the anterior pituitary gland and is the chief driver of statural growth during childhood [10]. Therefore, deficiency of this hormone can result in short stature condition.
In this patient, the laboratory results showed low FT4 and normal TSH level, which belonged to central hypothyroidism. Hypothyroidism is majorly divided into two categories, primary and secondary (central) hypothyroidism. Central hypothyroidism is when the thyroid gland itself is normal, and the pathology is related to the pituitary gland or hypothalamus. It is caused by a defect in the hypothalamic-pituitary axis [11].
This patient had not yet experienced wet dreams or any changes in his voice. No hair had grown either on his face or body. The volume of the testicle was still 2 ml each. His Tanner's stage was prepubertal (G1P1A1). In the male, delayed puberty is defined as a lack of increase in testicular volume at 14 years of age or a time-lapse of more than 5 years from the start to completion of genital growth. This patient has delayed puberty due to hypogonadotropic hypogonadism, based on the low level of gonadotropine hormone. We planned to give pubertal induction for this patient after optimizing his potential height with growth hormone therapy [12].
We did a bone age examination for this patient and it turned out that his bone age was 2 years and 8 months. Patients with growth hormone deficiency have a delay in bone maturation. The presence of hypogonadism with the consequent lack of circulating estrogens, androgens, and other pubertal hormones may also cause an important delay in bone maturation during the pubertal period [13].
We diagnosed this patient with multiple pituitary hormone deficiencies (MPHD) because we found a growth hormone deficiency, central hypothyroidism, and hypogonadotropic hypogonadism. MPHD may be idiopathic or result from genetically defined conditions. Congenital MPHD may be familial in 10% of cases, but it is usually sporadic. MPHD is characterized by impaired production of GH and one or more of the other pituitary hormones [14,15].
We did a brain MRI on this patient and the result was normal. MRI is a useful modality for delineating pituitary anatomy. MRI findings have a role in identifying children who are at higher risk for developing additional hormone deficiencies, as patients with MPHD have more frequent anatomical abnormalities of the pituitary than those with isolated GHD [16]. A study in Saudi Arabia in 2017 shows that most of the children with MPHD (6/11) showed anterior pituitary hypoplasia or (3/11) aplasia and 2/11 children with MPHD had normal MRI [17]. In addition, an MRI is performed to ensure the absence of an intracranial mass before giving growth hormone therapy [3].
Short stature due to MPHD is one of the causes of short stature due to endocrine disorders, which although it has a small percentage, is important because once diagnosed it can be treated with hormone replacement therapy. Growth hormone plays a role in all phases of growth, both prenatal and postnatal. Children who experience growth hormone deficiency will only experience a final height of around 130 cm. The goal of treatment with growth hormone is to improve the prognosis for adult height. From various recent studies, it can be seen that the final height results of children who receive growth hormone are much better than the predicted height at the start of treatment [3].
Treatment for short stature was given according to its etiology. Treatment with GH aimed to improve the prognosis of adult height. First, we gave recombinant human GH as hormone replacement therapy for growth hormone deficiency. Treatment of growth hormone could be started after confirming there was no intracranial mass by head CT Scan or MRI. Growth hormone (GH) was best given at night subcutaneously to adapt with endogen growth hormone production. The dosage given was 25-50 mcg /kg/day for prepubertal age and 100 mcg/kg/day for pubertal age. Treatment was given 6 days per week. The evaluation was done every 3-6 months. An increase in height and growth velocity was the most important indicator for evaluation. The treatment for a GH was stopped if the final height was reached or the epiphyseal plate was closed. Therapy is also stopped if the response to therapy is inadequate, namely if the increase in growth rate is less than 2 cm per year. In cases of growth hormone deficiency, growth hormone therapy should continue until adulthood, to optimize the metabolic effects of growth hormone and achieve normal peak bone mass. Children receiving growth hormone therapy require periodic monitoring. Usually done every 3 months to monitor growth with meaningful measurements. During the treatment evaluation, height, weight, pubertal status, examination of the injection site, and a comprehensive physical examination are carried out. The objective result of growth hormone therapy is an increase in growth rate and final height. Treatment is considered to provide a good response if linear growth increases > 2 cm per year. Increase in height as well as increase in growth rate are important evaluation indicators. Research on the safety of using growth hormone has been conducted by the Growth Hormone Research Society. In general, the side effects are minimal and only occur in less than 3% of cases. Side effects of growth hormone therapy include intracranial hypertension (pseudotumor cerebri), edema, slipped capital femoral epiphysis, worsening scoliosis, gynecomastia, hyperglycemia, and malignancy. During the period of growth hormone therapy, it is necessary to periodically check bone age every 12 months and thyroid function every 6 months as well as evaluate the side effects of treatment [3].
Growth hormone deficiency in children is mostly idiopathic and is treated with daily GH injections for a mean duration of 4 to 11 years. As a result, GH treatment is not only demanding on patients and their families, but it is also expensive. Furthermore, not all children benefit from GH treatment, and the poor response rate in GHD has been estimated to be between 10 and 30%. To minimize unnecessary daily injections and expenses, it is customary to monitor the response to GH therapy after one year to discover poor responders and revisit the diagnosis, adjust the GH dose, or discontinue treatment [18].
Thyroid hormone plays an important role in bone maturation in the prenatal and postnatal periods. Deficiency of thyroid hormone in childhood will cause slowed growth and retarded bone maturation. With levothyroxine treatment, growth will be seen to catch up so that they can reach normal height. Medication can be given in the morning or evening as long as it is given at the same time every day [3].
Short stature has so many differential diagnosis and etiologies, one of them is MPHD. Although MPHD was rare, we still have to be aware of the possibility of MPHD in a child with short-stature. Studying a case of children with MPHD can provide valuable insights into the diagnosis approach and management patient with MPHD, especially when facing patient with short stature.
Conclusion
We report a 13 years old boy who presented with short stature and delayed puberty. His height was under the third percentile for age. Tanner stage was prepubertal. Growth hormone stimulation test revealed a low level with a peak value of 0.124 ng/ml (normal level >7 ng/ml), thyroid hormone test showed low FT4 and normal TSH level, and gonadotropine hormone test showed low level of FSH, LH, and testosterone level. Working diagnosis was growth hormone deficiency, central hypothyroidism, and hypogonadotropic hypogonadism. This patient treated with growth hormone and thyroid hormone. The height increase 2.5 cm during 3 months of hormone replacement therapy. This article presents a rare case of a boy with short stature that turned out to be a multiple pituitary hormone deficiency (MPHD). MPHD has a small percentage, but it is important because if diagnosed it can be treated. Appropriate clinical examination and evaluation is very necessary so that an early diagnosis can be made and therapy is immediately given according to the etiology.
Acknowledgements
The authors would like to thank the Director of Dr. Soetomo General Acaedemic Hospital for supporting this study, and also they would like to appreciate all the Pediatrics staff in Department of Pediatrics for permission and support during the study.
Authors’ contributions
All authors contributed to data analysis, drafting, and revising of the article and agreed to be responsible for all the aspects of this work.
Conflict of interest
No potential conflict of interest was reported by the authors.
Funding
This case report did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Orcid:
N.M. Maya P. Wulandari: https://www.orcid.org/0009-0009-0121-1743
Nur Rochmah: https://www.orcid.org/0000-0002-9626-9615
Yuni Hisbiyah: https://www.orcid.org/0000-0002-1362-108X
Rayi K. Perwitasari: https://www.orcid.org/0000-0002-8699-4063
Muhammad Faizi: https://www.orcid.org/0000-0002-7009-4896
---------------------------------------------------------------------------------------
How to cite this article: N.M. Maya P. Wulandari, Nur Rochmah*, Yuni Hisbiyah, Rayi K. Perwitasari, Muhammad Faizi. A boy with short stature, be aware of multiple pituitary hormone deficiency. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(1), 111-121. Link: http://jmpcr.samipubco.com/article_183574.html
---------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
.png)
.png)
