Document Type : Original Research Article
Authors
Department of Environmental Health, Poltekkes Kemenkes Surabaya, Surabaya, Indonesia
Abstract
Kediri District is an endemic area, with dengue fever cases occurring every year. Kediri District has different topography, namely lowlands and highlands. The air temperature in the region ranges from 23 C to 31 C, but dengue fever cases occur evenly in the Kediri District area. Several factors influence the high number of Dengue Fever Cases, one of which is the presence of Aedes aegypti larvae in an area. The purpose of this study was to describe dengue fever cases, dengue fever risk areas and topography in Kediri District, East Java, Indonesia. This study was observational with cross sectional design. The object of the study was community health clinics in Kediri district, 37 areas. The variables studied were data on dengue fever cases, topography, and dengue risk areas. Data collection was done using interview and observation techniques. Data were displayed in the form of graphs and maps using Arcgis application. Results showed Kediri Regency 97% risk of dengue fever with percentage free of larvae of an area < 95%. From 37 public health services, Dengue fever cases are still the highest and all over the area scattered, the highest case in Public health service Pare observed from the topography of the Kediri Regency, 73% lowland.
Graphical Abstract
Keywords
Introduction
Indonesia is a tropical Asian country, has two seasons, namely the dry and rainy seasons, in one year having two seasons affects the density of Aedes aegypty mosquitoes. The population of Aedes aegypty mosquitoes will increase in the rainy season. Stagnant water caused by rainwater makes the development of Aedes aegypty mosquitoes increase higher than in the dry season. The correlation of increased development of Aedes aegypty mosquitoes is very high, this is associated with the incidence of dengue fever cases which are always high in the rainy season [1].
The development of the Aedes aegypty mosquito is not influenced by the topography of an area. Many cases of dengue fever occur in Indonesia which has different topography, namely lowlands, highlands such as hills and mountains. One of the regions in Indonesia with different topography is Kediri District. The topography in the region has an air temperature ranging from 23 C-31 C. The height of an area will affect the air temperature in the area. The air temperature decreases every hundred meters altitude, the air temperature will drop ± 0.27 °C [2].
Air temperature in each region affects the bionomics of Aedes aegypti larvae. The preferred temperature for breeding is ±29 C [3]. The presence of these larvae is a vector of dengue fever. High cases of dengue fever in an area, it is certain that the presence of larvae in the area is also present [4,5]. Dengue fever cases in Kediri District in 2021 increased again from the previous year. This study aims to describe dengue hemorrhagic fever cases by considering areas that have a risk of dengue fever seen from Topography in Kediri District, East Java, Indonesia.
Methods
This study was observational research in the field with a cross sectional design. The study was conducted in the Kediri District area as many as 37 public health services in 2022. The variables studied were data on dengue fever cases, regional topography and dengue risk areas obtained by making direct observations in the field at the homes of dengue fever sufferers. Data collection was done using interview and observation techniques in the community. Data is displayed in the form of graphs and maps using Arcgis application.
Penentuan areas at risk cases of DHF
Conducting a dengue vector survey to determine dengue risk areas in an area is by calculating the larval index based on the ratio of the number of houses declared larvae-free compared to the number of houses examined. The indicator in determining a larval-free area is if the larval index calculation result is ≥ 95%. Areas with a larval index ≥ 95% are categorized as areas not at risk of dengue fever transmission.
Spaasial analysis
Data were analyzed in spatial form and displayed in a geographic information system (GIS) in the form of maps using ArcGis software.
Ethical Approval
This research has been approved by the Surabaya Health Polytechnic Health Research Ethics Committee with registration no. EA/1137/KEPK-Poltekkes_Sby/V/2022.
Results
Dengue fever cases in Kediri district in 2022 were spread throughout the working area of the Public Health center. The highest cases were in the Pare community health clinic area with 61 cases of DHF and the lowest in the Pelas community health clinic area with 3 cases (Figure 1).
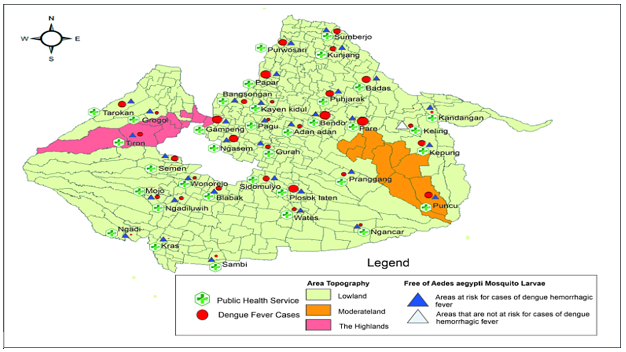
Based on the spatial analysis of the area, the mapping of the number of dengue hemorrhagic fever cases with the potential for transmission seen from the dengue vector density indicator, namely the larval index, can be seen in Figure 2. The results of the calculation of the larval index used to determine areas that have the potential for dengue transmission, there are 97% of areas where dengue vector density is found and 3% of areas not at risk of dengue transmission, namely the area in the Keling community health clinic. Keling public health service is an area not at risk of dengue fever transmission, seen from the dengue hemorrhagic fever cases in that area are still high at 19 cases. Almost all areas in Kediri District have the potential for dengue fever transmission. Dengue Fever cases are highest in the Pare public health service with 61 cases, but the Flick Free Rate of 75% is still above the Purwoasri public health service. The topography of the area in Kediri District is divided into three: lowland 0-400 m above sea level, medium 400-700 m above sea level, and high ≥700 m above sea level. Most of the Kediri District area is in the lowland area of 73%, and 5% is highland, namely the Puncu Public Health Service, while 22% is mediumland, namely the Ngancar, Plosoklaten, Pranggang, Keling, Kepung, Bendo, Pare, and Sidorejo Public Health Services. The distribution of dengue hemorrhagic fever cases and dengue vector density in terms of topography can be seen in Figure 3.
Public health service Puncu is a highland, with a larval index < 95% with a high number of DHF cases at 40 cases. Keling Public Health Service is a medium altitude area, with a larval index ≥ 95% with 19 cases of DHF. The highest number of DHF cases in Kediri District was found in Pare Public Health Service with 61 cases with a larval index < 95%.
Discussion
Kediri District is a dengue fever-endemic area, as all areas in Kediri district have the potential risk of dengue fever. The presence of Aedes aegypti mosquito larvae is still present in every region, and there is a very strong relationship between the presence of larvae and dengue fever cases in an area. The relationship between the presence of mosquito larvae and the incidence of dengue fever, not only in Kediri District but in other areas, but it is also evident, such as Boyolali, Sawit District, and Surabaya City [6,7].
Dengue fever is influenced by the density of Aedes aegypti mosquitoes, while the density of Aedes aegypti mosquitoes depends on environmental sanitation conditions. Poor environmental sanitation conditions provide opportunities for Aedes aegypti mosquito larvae to develop well. Aedes aegypti mosquitoes need clean water to lay eggs, but in urgent conditions, they can lay eggs in dirty water despite its high organic matter content, unless the dirty water contains ammonia, such as laundry wastewater [8]. The density of Aedes aegypti mosquito larvae can continue to grow, influenced by the place of egg laying in clean water, such as water reservoirs preferably dark in color and made of plastic, with room temperature of 29.54 °C and humidity 76.29% [3], Poor sanitation conditions in the home environment, due to many water reservoirs in the home, such as animal drinking water containers, used bottles and buckets, uncovered barrels, bathtubs, flower vases, pots, or other used items[9-11].
The presence of larvae in Situbondo district is proven to be a vector carrier of dengue virus-causing dengue hemorrhagic fever (DHF). This is proven every year because dengue fever is always present in the region. One of the reasons why the Aedes aegypti mosquito larvae as carriers of dengue virus cannot be destroyed is the way of control carried out in the region using chemical control, which is carried out continuously and over a long period of time. The larvae of Aedes aegypti mosquitoes in the area have proven to be resistant to the organophospate insecticide temephos [12]. Control of adult Aedes aegypti mosquitoes is also carried out chemically by fogging using malthion insecticides made from the active organophospat group, so that both larvae and adult mosquitoes are continuously using insecticides in one class. This causes adult mosquitoes and larvae to become resistant to insecticides of that class [13,14].
Kediri District is topographically divided into three plains: lowland, sandy, and highland. The percentage of lowland areas out of 37 areas assisted by the public health service is 73%; the sea plains are 22%; and the highlands are only 5%. The spread of dengue fever and the presence of Aedes aegypti mosquito larvae are spread from lowland to highland areas. The distribution of dengue fever cases based on the altitude of Kediri District also occurred in 2021, indicating that Kediri District is a dengue fever-endemic area. There is no difference in dengue fever cases between the lowlands and the highlands; the region has the same number of dengue fever patients as the highlands [14]. This result is different from the distribution of dengue fever cases in Manado City, Malala Subdistrict, where dengue fever sufferers in lowland areas are far more than in areas in the southern and highland categories [15]. Sleman Regency has a larva-free rate of almost all sub-districts with a value of <95%, meaning that there are still many Aedes aegypti mosquito larvae, and positively in the Aedes aegypti mosquito larvae there is dengue virus, proven by the presence of dengue fever sufferers in the area. Patients with dengue fever in Sleman Regency are spread out in low to highland areas, which distinguishes the highlands with fewer cases than the lowlands [16]. Aedes aegypti mosquitoes breed well in tropical and sub-tropical climates that have air temperatures ranging from 18 °C to 30 °C. Aedes aegypti mosquitoes lay eggs in areas that have warm temperatures; breeding only takes two days, but in areas with cold temperatures, the Aedes aegypti mosquito takes ± a week. Egg hatching is also influenced by air temperature; the higher the air temperature, the lower the humidity. This condition will cause the hatching of eggs to decrease, so that relatively fewer larvae are formed. A decrease in pupation occurs when the room temperature is ≥30 °C [17,18]. Increasing temperatures in the Americas also decreased the capacity of the Aedes aegypti mosquito [19]. The growth of Aedes albopictus mosquitoes is well developed in the Alps of northern Swiss cities[20]. The results of resistance testing research in Kediri district, East Java, Indonesia, showed that Aedes aegypti mosquitoes experienced resistance to malathion insecticide [13]. This is why dengue fever cases are still high every year. The increase in dengue vector density in tropical countries is very high and unavoidable, especially during the rainy season. Efforts are made for effective mosquito population control by larvasidating water reservoirs and implementing the government's appeal, namely draining and tightly closing water reservoirs and recycling used goods. The high incidence of dengue fever is because people do not implement the government's appeal to close, drain water reservoirs and process used material [21,22]. These activities can be carried out with the movement and cultivate mosquito breeding behavior [23]. It is different if the eradication of mosquito nests by repeated and too frequent use of malation insecticide will cause resistance. Therefore, it is recommended to replace mosquito eradication by fogging using insecticides from a different class of pyrotroids such as chypermetrin. The results of resistance testing of Aedes aegypti mosquitoes in Kediri District to chypermetrin insecticide have not experienced resistance to the insecticide [14].
Conclusion
The topography of Kediri District is mostly 73% lowland; 97% of areas in Kediri District have a larva-free rate of <95%, meaning that the area is at risk of dengue fever cases. Dengue fever cases are spread throughout Kediri District, both lowland and highland, with the highest cases in the Pare public health service area. The community is advised that in an effort to control vectors independently, they are required to carry out government programs, namely draining and tightly closing water reservoirs, recycling used goods, and conducting larvicides in water reservoirs.
Acknowledgments
The authors would like to thank the Kediri District Health Office and the Surabaya Health Polytechnic for providing support in this research process.
Author's Contribution
All authors have contributed equally to the completion of this research. All authors approve and validate the submitted manuscript.
Conflict of Interest
The authors declare that there is no conflict of interest in this manuscript.
Orcid:
Demes Nurmayanti*: https://orcid.org/0000-0003-1030-6313
Ngadino Ngadino : https://orcid.org/0009-0003-6980-7056
Marlik Marlik: https://orcid.org/0000-0002-5812-1521
Slamet Wardoyo: https://orcid.org/0000-0003-3936-1893
------------------------------------------------------------------------------
How to cite this article: Demes Nurmayanti*, Ngadino Ngadino, Marlik Marlik, Slamet Wardoyo , Spatial analysis of dengue fever by region and topography in kediri regency, east java, Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(3), 327-333. Link: http://jmpcr.samipubco.com/article_184845.html
------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
