Document Type : Original Research Article
Authors
- Zohreh Azarkar 1
- Ali Mohammad Zadeh 2
- Roohie Farzaneh 3
- Mahdi Foroughian 3
- Behrang Rezvani Kakhki 3
- Maryam Sobhani 4
- Molood Fogerdi 5
- Maryam Ziyaei 6
- Fatemeh Maleki 5
1 Department of Infectious Diseases, Infectious Diseases Research Center, Birjand University of Medical Sciences, Birjand, Iran
2 Student research committee, Birjand University of Medical Sciences, Birjand, Iran
3 Department of Emergency Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
4 Department of Emergency Medicine, North Khorasan University of medical sciences, Bojnurd, Iran
5 Department of Emergency Medicine, Birjand University of Medical Sciences, Birjand, Iran
6 Department of Emergency Medicine, Zahedan University of Medical Sciences, Zahedan, Iran
Abstract
Introduction: Understanding the interplay of paraclinical factors in individuals with COVID-19 is crucial for predicting disease prognosis. This study aims to explore the correlation between lymphocyte count, C-reactive protein (CRP) serum levels, CT scan findings, and the ultimate outcome in patients with COVID-19 pneumonia at Valiasr Hospital in Birjand.
Methods: Conducting a retrospective analysis, this study investigated 258 COVID-19 patients aged 14 and above, who sought medical attention at Valiasr Hospital in Birjand city in 2020. The research meticulously documented patients' demographic details encompassing gender, age, education level, underlying health conditions, lymphocyte count, and other pertinent information. CT scan findings, the ultimate patient outcomes, and serum levels of CRP were systematically recorded and comprehensively analyzed using a study checklist. This comprehensive examination aims to provide a detailed retrospective understanding of the multifaceted factors influencing COVID-19 outcomes among patients in Birjand.
Findings: The average age was 61.06±20.06 years. 50.8% of patients were male. 10.9% of patients died. The average number of lymphocytes did not differ significantly according to the severity of lung involvement (P=0.291), but the average number of WBC (P=0.031), the percentage of lymphocytes (P=0.047) and CRP (P<0.001) was significantly different from each other according to the severity of the conflict. CRP levels in discharged group were significantly lower than dead, ward and ICU admitted ones (P<0.05). CRP levels were significantly lower in without lung involvement patients than all other groups except the mild involvement group (P<0.05).
Conclusion: Elevated serum levels of CRP and white blood cell count, coupled with a decrease in lymphocyte percentage, were linked to more lung involvement. Furthermore, a reduction in both the number and percentage of lymphocytes correlated with a more severe condition as well as the high CRP levels’ effect.
Graphical Abstract
Keywords
Main Subjects
Introduction
At the end of 2019, news emerged regarding the spread of a novel viral disease in a Chinese city. COVID-19 epidemic initially identified in Wuhan, China, and has since evolve into a worldwide pandemic [1,2]. The pathogen responsible for this disease, named SARS-CoV-2, rapidly resulted in widespread transmission due to its high contagiousness [3]. Transmission primarily occurs through respiratory droplets from infected individuals, contaminated surfaces, or inanimate objects. The incubation period typically spans 2 to 14 days, during which patients can be infectious [4]. The disease's severity varies, with 81% of cases being mild, 14% categorized as severe (with symptoms like shortness of breath or lung involvement in imaging), and 5% classified as critical (characterized by respiratory failure, shock, or the malfunctioning of many organs) [5]. The total mortality rate stands at 2.3%, with most fatalities occurring among elderly patients or individuals with underlying health conditions [6]. Accurate diagnosis of viral pneumonia through chest CT scans plays an important role in managing suspected COVID-19 cases [7]. However, there is ongoing debate about the use of CT scans for diagnosing and managing the disease [8]. Severe cases or complications often require specialized care, including admission to intensive care units (ICU) for patients requiring ventilatory support. Unfortunately, there were gaps between the demand for ICU beds and their availability during the peaks of disease [9]. In addition, the expenses for ICU services include 39% of the overall expenditure on drugs, 25% on equipment, and 13% on laboratory research in hospitals [10]. Scientists are currently trying to discover a conclusive treatment for COVID-19, and trials are now being conducted on some antiviral medications, anti-inflammatory, and antimalarial drugs, and even herbal medications [11]. Different waves of epidemic had also different clinical presentations in patients [12]. Clinical diagnosis primarily relies on epidemiological history, clinical symptoms, nucleic acid testing, CT scans, IgM/IgG immune detection, ELISA, and blood cultures [13]. Common initial symptoms include fever (99%), dry cough (59%), fatigue (70%), and shortness of breath (31%) [14]. Laboratory tests often reveal abnormalities in leukocyte counts, lymphocytes, and CRP levels [14-17]. Coagulopathies are also possible among these patients [17]. In addition, due to the inflammation caused by the virus, the CRP test is also important, which is positive in most patients. According to the completed study by Zheng et al. in 2020, there is a relationship between natural killer cells and T lymphocytes, so that it is significantly reduced in patients with COVID-19 [18]. Huang et al. studies showed an interconnection between the count of lymphocytes and the tensity of the COVID-19, so the number of lymphocytes decreases with the increase in the severity of the disease [19]. Considering the above information and the fact that COVID-19 is a global societal issue, research related to it should be conducted to better manage the disease. Even though some studies have been carried out in certain parts of the world, it is advisable to compare patients with different races and genetics to enhance our understanding of this virus. Therefore, this research aims to investigate the association between lymphocyte numbers, CRP serum levels, CT scan results, and the final outcome of the disease in patients with COVID-19 referred to Valiasr Birjand Hospital.
Methods
This study is a retrospective study on COVID-19 patients admitted to Valiasr Hospital during the study period, whole 2020. The study population includes patients older than 14 years old with symptoms in favor of COVID 19 who referred to Valiasr hospital in Birjand city, whose PCR test result of COVID-19 was positive or the findings of CT scan of the lung were highly suggestive in favor of COVID-19. Sampling was done after obtaining permission from the Ethics Committee of Birjand University of Medical Sciences (IR.BUMS.REC.1400.263). Inclusion criteria included Age more than 14 years, patients who visited Valiasr Hospital with symptoms of COVID-19 and had a positive COVID-19 PCR test result or had a highly suggestive lung CT scan in favor of COVID-19. Exclusion criteria also included having underlying diseases such as diabetes, heart and lung disease (COPD), patients who have non-covid inflammatory or infectious involvement in any part of the body, patients who have bone marrow involvement with the category of lymphocyte involvement, taking corticosteroids and any defect of the immune system. In this study, the goals of the research informed the development of a checklist and the necessary information was recorded from the patients' files or the patients themselves. Demographic information of the patients including gender, age, education level, underlying diseases, lymphocyte count and other information including the CT scan findings of the patients, finally the final outcome of the patient and the serum level of CRP were recorded in the checklist. The findings of the CT scan at the arrival of the patients were calculated as follows given that the country's instructions for the outpatient and inpatient prescription of COVID-19 in September 2019:
- The number of segments and lobes with ground glass design 2. The number of segments and lobes with consolidation 3. The number of segments and lobes with crazy paving 4. Score of level of lung involvement was calculated as follows given that the country's instructions for outpatient and inpatient COVID-19 in September 2019 (first, the level of involvement in each lobe was scored):
0: no involvement in each lobe, 1: zero to 25% involvement, 2: 25 to 50% involvement, 3: 50 to 75% involvement, 4: 75 to 100% involvement of each lobe. Then the resulting number is multiplied by 5 for the lower lobe on both sides, multiplied by 3 for the upper lobe on both sides, and multiplied by 2 for the middle lobe and lingula and finally added together, which was a number between 0 and 80 (parameters that depend on the number of segments in each lobe). The intensity of the conflict was divided as follows: Group one: mild without lung involvement Group two: mild with less than 10% involvement [1-16].
Group three: Medium with involvement between 10 and 40 percent (number 32-17).
Group four: severe with involvement more than 40-75% (60-33). Group five: crisis with more than 75% conflict (number above 60).
The information regarding lymphocyte cell count and CRP serum levels was determined based on blood samples taken from the patients at the time of referral. The CRP serum levels were categorized into four groups according to the national criteria for diagnosing and treating COVID-19 in both outpatients and inpatients as of December 2020. These criteria also followed the protocols outlined by the Scientific Committee of Khorasan Razavi Corona Headquarters in 2019 for the identification and management of COVID-19 in individuals receiving care outside of a hospital setting, as well as those admitted to a hospital (CRP normal range considered to be less than or equal to 6).
Group one: 6 and less, group two: between 7 and 12, group three: between 13 and 40, group four: between 41-100, group five: more than 100.
Data analysis was done using SPSS version 21 software and descriptive and inferential statistics (Kruskal, Wallis, Mann-Whitney and Chi-square) at a significance level of P<0.05.
Results
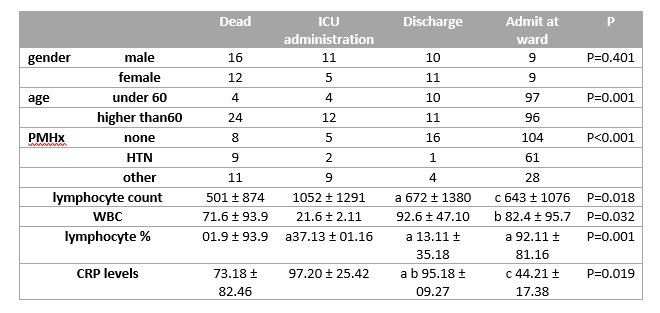
A total of 258 patients with an average age of 61.06±20.06 years participated in this study. 50.8% of patients were male. 34.5% of illiterate patients and 51.6% of patients had no underlying disease. 10.9% of patients died and 8.1% of patients were discharged. Also, 9.7% of patients without involvement and 14.3% of patients had critical severity (Table 1).
Among gender categories, males had higher numbers in the Dead and ICU Administration outcomes, while females show relatively balanced outcomes and gender had no differences among study groups (P=0.402). Regarding age, patients under 60 tend to be more prevalent in the admit at ward category, while those over 60 are more commonly observed in the Dead category. So, most critical cases (dead and ICU hospitalized) were older than 60 (P<0.001), (Table 1). 9.7% of patients had CRP serum levels less than 6 and 48.4% had serum levels between 100-41. Also, 59.3% of patients had lymphocytes below 1100 and 40.7% had lymphocytes above 1100. 89.9% of patients had ground glass opacity, 65.9% had consolidation opacity, and 8.5% had crazy paving opacity. Average number of lymphocytes 1093 ± 670, lymphocyte percentage 11.08 ± 16.14, WBC count 5.41 ± 8.57 and CRP It was 21.28 ± 38.46. In comparison of patients based on the outcome, significant differences were seen in lymphocyte count of discharged and dead patients, with higher lymphocyte counts in discharged group (P=0.001) and admitted patients in ward had significantly higher lymphocyte count than dead ones (P=0.001). Also, significant differences were shown in WBC count of admitted in ward and ICU patients, with higher WBC counts in ICU group (P=0.032). Also, there were significantly higher lymphocyte percent of admitted in all groups than dead group (P<0.001). CRP levels in discharged group were significantly lower than dead, ward and ICU admitted ones (P<0.05).
As shown in Figure 1. CRP levels were significantly lower in without lung involvement patients than all other groups except the mild involvement group (P<0.05). Individuals with moderate involvement show a significantly higher mean CRP level.
(38.8±20.02 mg/L) compared to those without involvement (26.36±18.93 mg/L). Furthermore, the CRP levels in individuals with severe involvement (46.55±19.61 mg/L) and those with critical involvement (46.43±19.47 mg/L) exhibit statistically significant differences when compared to the mild involvement group (30.86±21.45 mg/L).
Discussion
In the current investigation, the average age of patients was 61.06 ± 20.06 years. However, our findings differ from those reported by Mehrtash et al. [20], Tian et al. [21], Alian et al. [22]. Conversely, Bagheri et al. [23] noted an average age of 71.13 ± 8.6 years, indicating a discrepancy with our results, possibly attributed to variations in sampling methods and data collection. Notably, Matos et al. [24] reported an average patient age of 63.5 years, aligning with our study. Regarding gender distribution, the majority (50.8%) of patients in our study were men, a pattern consistent with findings in studies by Mehrtash et al. [20] and, Dadgari et al. [25]. Due to the fact that men are responsible for providing livelihood for their families and their workplace is outside the home environment, the rate of infection of men with COVID-19 was higher than that of women. Also, because men went to health centers later than women and had less rest, they visited health centers more intensively. In the present study, 10.9% of patients died and 8.1% of patients received their discharge from the hospital. In the study by Akhavizadegan et al. [26] it was equal to 23%, which was inconsistent with our study. Among the reasons for this inconsistency, we can highlight the disparity in the study duration and the criteria for participant selection. It can be stated that proper information has been provided to the population living in Birjand compared to the cities where the patients lived in the above two studies, that the patients had referred to the medical centers earlier and had a lower death rate. Moreover, the current conditions suggest that the disease monitoring and diagnosis system in Birjand may be comparatively weaker than in the aforementioned cities. In the current study, 9.7% of patients had no involvement, 26% had mild involvement, and 38% had severe involvement. According to the study by Alian et al., the severity of lung involvement was 22% for patients with mild involvement, which was consistent with our study. Additionally, this study reported that the severity of severe involvement in the patients under study was 25%, which did not align with our findings [22]. Among the reasons for this inconsistency, we can point to differences in society, time, and geographical region. In the present study, 9.7% of patients had a serum CRP level less than 6, while 64.8% had a serum level of more than 100. Additionally, 40.7% had a lymphocyte count above 1100. In a study by Mohammadi et al. [27], it was asserted that lymphopenia was a common finding in patients with COVID-19, a result consistent with our study. According to the results of the present study, the most common type of opacity (with a frequency of 89.9%) was ground glass opacity, followed by consolidation opacity and crazy paving opacity. In a study by Dalirrooy Fard et al., it was stated that the most common type of opacity in patients was ground glass opacity, which was consistent with our study [28]. In the study conducted by Kwee et al., it was reported that the most common opacity observed in the CT scans of patients with COVID-19 was ground glass opacity, which was consistent with our study [29]. Therefore, based on the results of the present study and other studies, the most important CT scan symptom for diagnosing ground glass opacity is observed in the early stages of COVID-19 in patients and can be used as a diagnostic tool alongside PCR when diagnosing the disease. The mean number of lymphocytes did not differ significantly based on the severity of lung involvement. However, there was a significant difference in the average number of WBC, percentage of lymphocytes, and CRP levels among patients with different degrees of involvement. Francone et al.'s study reported a correlation between the mean serum CRP level and the severity of lung involvement (CT scan score), which was in line with our findings. Therefore, it can be concluded that the CT score has the potential to predict the final outcome of SARS-CoV-2 patients. The average number and percentage of lymphocytes, WBC count, and serum CRP levels significantly varied based on the final outcome of the patients. Mohammadi et al. [27] reported that the mean WBC count and lymphocyte numbers significantly differed with respect to the final disease outcome, consistent with our study. Matos et al. found that the average serum CRP level and lymphocyte percentage were related to the final outcome of the patients, in line with our findings [24]. Luo et al. also noted a relationship between white blood cell count, CRP levels, lymphocyte count, and disease outcome, consistent with our study [30]. The distribution of the final outcome of patients significantly varied based on the severity of pulmonary involvement, age group, and underlying disease. However, there was no significant difference in the distribution of disease outcomes based on the gender of the patients. Assiri et al. [31] reported a significant relationship between increasing age and the mortality rate of patients with COVID-19, consistent with our study. Increasing age is associated with various diseases in elderly patients, leading to compromised immune system responses, organ dysfunction, accelerated inflammation, and increased mortality in COVID-19 patients [32]. The immune system in the elderly exhibits heightened reactivity due to increased expression of genes related to inflammation. However, as individuals age, their immune system's adaptability becomes impaired, weakening their overall immune response. This weakening contributes to increased virus pathogenicity, leading to more severe diseases and higher mortality rates [33]. Zhou et al. [34] reported that the distribution of mortality rates among COVID-19 patients based on the presence of underlying diseases differed significantly, which aligns with our study. Akhavizadegan et al. [26] also found a significant difference in mortality rates based on the presence of underlying diseases, consistent with our findings. However, our study did not find a significant difference in mortality rates based on specific conditions like respiratory disease, kidney disease, and diabetes. This discrepancy could be attributed to differences in inclusion criteria and study populations. Diabetes is known to disrupt the immune system and its response, reducing immune function by impairing neutrophil chemotaxis, monocyte antibacterial activity, and phagocytosis, thereby increasing susceptibility to infections [34,35]. Additionally, diabetes can lead to disturbed inflammatory responses to cytokines, potentially contributing to increased severity and mortality in COVID-19 patients [34,35]. Respiratory system damage can reduce respiratory function and increase susceptibility to viral infections. Patients with cardiovascular diseases, such as high blood pressure and heart disease, may experience higher mortality rates due to cardiovascular weakness induced by stress and chronic inflammation [36]. In summary, chest CT scans are a common imaging tool for diagnosing pneumonia and can be a valuable tool for prognosis. However, it's important to emphasize that CT scans are neither necessary nor sufficient for COVID-19 diagnosis and prognosis [36,37].
As COVID-19 patients experience prolonged consequences [38,39], further follow up of inflammatory factors are needed. Also, age is an important factor that widely affects the mortality rate and in our study, the effect of age should be considered along with the main hypothesized factors.
Conclusion
In the present study, the percentage of lymphocytes, the number of WBCs and the serum level of CRP were related to the severity of lung involvement of the patients and also the final outcome of the patients, so with the increase of the serum level of CRP and the number of white blood cells and the decrease of the percentage of lymphocytes, the level of lung involvement It was significantly more. Also, with a decrease in the number and percentage of lymphocytes, and an increase in the serum level of CRP and WBC, the final outcome of the patients was worse.
Conflict of interest
None.
Authors' contributions
All authors contributed toward data analysis, drafting, and revising the article and agreed to be responsible for all the aspects of this work
Orcid:
Zohreh Azarkar: https://www.orcid.org/0000-0001-5967-5836
Ali Mohammad Zadeh: https://www.orcid.org/0009-0007-5038-5729
Roohie Farzaneh: https://www.orcid.org/0000-0002-0892-1555
Mahdi Foroughian: https://www.orcid.org/0000-0002-3944-9361
Behrang Rezvani Kakhki: https://www.orcid.org/0000-0003-3715-6618
Maryam Sobhani: https://www.orcid.org/0000-0001-8621-3186
Molood Fogerdi : https://www.orcid.org/ 0000-0002-5476-4001
Maryam Ziyaei: https://www.orcid.org/0000-0003-1693-6818
Fatemeh Maleki *: https://www.orcid.org/0000-0002-6823-5151
---------------------------------------------------------------------------------------
How to cite this article: Zohreh Azarkar, Ali Mohammad Zadeh, Roohie Farzaneh, Mahdi Foroughian, Behrang Rezvani Kakhki, Maryam Sobhani, Molood Fogerdi, Maryam Ziyaei, Fatemeh Maleki *, Prognostic value of lymphocytes counts, serum CRP levels, and lung CT scan findings and the final disease outcome in COVID-19. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(3), 334-343. Link: http://jmpcr.samipubco.com/article_184881.html
---------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
