Document Type : Original Research Article
Authors
Department of Orthopedic and Traumatology, Faculty of Medicine, Universitas Airlangga, Dr. Soetomo General Academic Hospital, Surabaya, Indonesia
Abstract
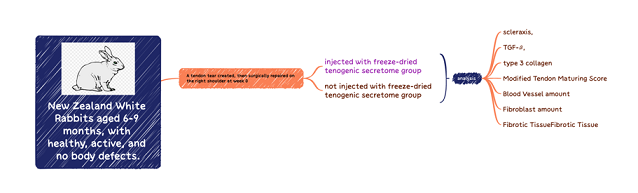
Rotator cuff tear is the major cause of morbidity which affects over 40% of patients aged 60 years and older. Surgical repair is often unsuccessful and has high complications. Tissue engineering therapies, such as applying Mesenchymal stem cells (MSCs) secretomes, have shown beneficial effects on tendon repair. This study aims to assess the effect of secretome application on rotator cuff tendon tears by examining changes in transforming growth factor beta (TGF-β), Scleraxis, and Collagen type III levels. A total of 20 post-injured supraspinatus tendon New Zealand white rabbits were divided into 2 groups: injected with of frozen-dried tenogenic secretome (treatment group) and no treatment (control group). Histologic evaluation on the repaired site was conducted on the second and the fourth weeks; analysing immunohistochemistry (IHC), TGF-β, Scleraxis, collagen type III levels, modified tendon maturing score, blood vessel, fibroblast, and fibrotic tissue. Immunoreactive Score (IRS) result for TGF-β, Scleraxis, and collagen type III on treatment group were moderate. Meanwhile, IRS result for control group was a mix of mild and moderate. Compared to the control group, a significant difference was found (p<0.05). Histologically, Modified Tendon Maturing Score, amount of blood vessel, and fibroblast were found to be significantly higher (p<0,05) in treatment group. Meanwhile, fibrotic tissues were significantly lower (p<0,05). Secretomes promote the healing of specific tissues such as tendons in vitro and in vivo. TGF-β is crucial for collagen synthesis, while scleraxis facilitates tendon-bone attachment. Collagen type III initiates tendon repair, requiring increased blood vessel and fibroblast growth and lower fibrotic tissue.
Graphical Abstract
Keywords
Introduction
Rotator cuff tendon tears are a significant cause of pain, reduced shoulder function, and weakness, affecting over 40% of patients over 60 years old. In the United States, approximately 30,000 to 75,000 tendon repairs are performed annually [1]. Tendons are difficult to heal due to their hypo-vascular nature, leading to scar tissue and weaker ectopic bone [2]. Despite the development of surgical techniques for tendon repair, failure, and complications rates remain high even after therapy [3].
Tissue engineering strategies have been developed to create functional replacements or accelerate natural healing of tendon defects. Applying stem cells directly to the injured site provides new precursor cells that proliferate and differentiate into new cells - but this has limitations, including low concentration of cells in the injured site and the long process of making the composite [4].
Recent studies are prioritizing cell therapy using mesenchymal stem cell (MSCs) secretomes instead of providing the stem cell itself to the injured site. Secretome MSCs significantly reduce the number of cells needed for transplantation and increase the ratio of production quantities through dynamic control of laboratory conditions (bioreactor). This allows for phenotypic adjustment and therapeutic potential [5,6]. Several bioactive molecules play a crucial role in coordinating cellular responses during tendon healing. Growth factors like insulin-like growth factor-I (IGF-I), Transforming growth factor beta (TGF-β), basic fibroblast growth factor (bFGF), platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), Bone morphogenetic proteins (BMP), Scleraxis (Scx), collagens, and connective tissue growth factor (CTGF) contribute to different stages of healing process. Other bioactive molecules, such as growth regulators and extracellular matrix (ECM) degradation enzymes like matrix metalloproteinases (MMPs) and their inhibitors- tissue inhibitor metalloproteinases (TIMPs), are also essential for tendon repair [7].
Despite the secretomes potential for tendon healing, their specific role remains unelicited. This research aims to assess the effect of secretome application on rotator tendon cuff tear by examining changes in TGF-β, scleraxis, collagen type III Levels, and histological evaluation.
Materials and methods
This study was a true experimental with a randomized post-test only with a control group design. In this study we divided the sample into two groups, namely the control group (not injected with freeze-dried tenogenic secretome) and treatment groups (injected with freeze-dried tenogenic secretome). Grouping is decided by randomization using lottery. Each rabbit was given a number, and then a draw was carried out for each group with a total of two groups. All animal procedures were in accordance with The Animal Care and use Committee of Veterinary Faculty Medicine of Airlangga University (Ethical Clearance No. 2.KEH.151.09.2023). The study subjects were the injured supraspinatus tendon of adult New Zealand white rabbits. To fit the sample, the rabbit must meet the inclusion criteria of male sex, adult aged (6-9 months), have an average weight of 2000 ± 500 grams, no body defect, and is healthy yet active. Meanwhile, rabbits which are aged less than 6 months or more than 9 months and rabbits which suffered from illness or other infections were excluded from this study. Briefly speaking, tendon tear was created on the right shoulder surgically on week 0. After that, we repaired the torn supraspinatus tendon using size no. 8-0 end-to-end, and then the freeze dried tenogenic secretomes were injected into the tendons for the treatment group and repaired the tendons. Four weeks after injection, the rabbits were terminated and the supraspinatus tendons were taken to make histological preparations. The minimum number of samples was calculated using statistical formula and it was found that a minimum of 10 samples was required for each group. Histologic evaluation on the repaired site was conducted on the second and fourth week. Modified Tendon Maturing Score, amount of fibroblast, amount of blood vessel, and fibrotic tissue were noted. The scleraxis level, TGF-β, and collagen type III would also be analysed from each sample four weeks after treatment. The collected data will be analysed statistically using the SPSS 26 program. Normality is firstly tested using Saphiro-Wilk test. If normal, independent t-test will be used to test for significancy. Mann-Whitney is used as alternative non-parametric test. p<0.05 will be accepted as significant. In this study, bivariate ordinal data were obtained so that a test would be carried out using the Mann-Whitney.
Rotator cuff tear preparation
- Rabbits were imported from breeders who understood animal health. Rabbits with a body weight of 2000-2500 grams were used. They were placed in cages measuring 50 x 70 cm in a special room for rabbit placement. The rabbits were acclimated to the experimental animal laboratory's ambient conditions for a period of 7-10 days. They were provided with unlimited access to water using the ad libitum method, and their daily food intake consisted of 300 grammes of pellets. The rabbit excrement is cleaned each morning. Infirmed rabbits were precluded from being placed in the enclosure. Nevertheless, in the case of a slight sickness, the rabbit will receive either vitamins or antiparasitic medication.
- The rabbits were administered ketamine (40 mg/kg) and xylazine (10 mg/kg) intramuscularly in the supraspinatus area for anaesthesia induction. Subsequently, a maintenance dose of 10 mg/kg was administered intramuscularly if the rabbits exhibited a reaction. Subsequently, the rabbits underwent a period of fasting lasting up to 6 hours after the surgery. The rabbit's forelimbs were depilated using a razor, leaving a 5 cm space from the operation field. The treated region was disinfected with a 10% solution of povidone iodine, followed by the use of a sterile serviette to restrict the operative field.
- The area to be treated for the injury model is at the base of the hind limbs of the rabbit, which is 1 cm proximal to the muscle-tendon junction of the supraspinatus muscle. An incision is made in the skin and deepened layer by layer until it reaches the muscle layer. Tendon excision was carried out with a length of 1cm, a width of 0.5 cm, and a depth of 0.5 cm.
- As a marker, a knot is given using a nonabsorbable monofilament thread measuring 3.0 - 5 mm proximal and distal from the incision site to facilitate the identification of the incision site when observing later. An incision was made in the tendon of the right forelimb to be given the secretome injection treatment, and then the rabbits were taken care at the Faculty of Veterinary Medicine Airlangga University. The freeze-dried tenogenic secretome was isolated and made at the cell tissue bank of Dr. Soetomo General Academic Hospital.
- Sampling of muscle tissue in the treatment area was carried out at the end of the fourth week according to the division of groups that had been determined sterilely. Network retrieval is carried out between the two marker nodes that have been previously given. The collected tissue is put into a container that has been labelled and filled with formalin buffer.
Analysis of scleraxis, TGF-β, and collagen type III through immunohistochemical analysis
The glass objects that had been deparaffinized were then stained using IHC reagents for respective parameter: scleraxis, TGF-β or collagen type III. The glass objects for each parameter were stained using antibodies and then rinsed using Phosphate-buffered saline (PBS) for 3x5 minutes. The object glass was counterstained using 4′,6-diamidino-2-phenylindole (DAPI), and then incubated for 10 minutes and then rinsed again with PBS for 3x5 minutes. The amount of scleraxis, TGF-β or collagen type III was evaluated under the microscope by estimating the intensity and averaging the scleraxis percent of, TGF-β or collagen type III clusters that were visible in the six evaluated segments. Result is classified based on immunoreactivity score (IRS) classification into mild, moderate, and strongly positive.
Analysis of modified tendon maturing score, amount of fibroblast, amount of blood vessel, and fibrotic tissue
Analysis of Modified Tendon Maturing Score was done based on previous scoring method [7]. Meanwhile, amount of fibroblast, blood vessel, and fibrotic tissues were done by manual calculation counting on the detectable fibroblast, blood vessel, and fibrotic tissue on histological preparation stained with haematoxylin eosin. Calculation was based on the average of countable fibroblast, blood vessel, or fibrotic tissue on at least five viewing fields.
Results and discussion
Evaluation result of collagen type III, TGF-β, and scleraxis for the control and treatment groups are elaborated. At glance, it appears that tissue exposed to tenogenic secretomes shows increased expression in all three parameters (Figure 1).
Based on the IRS, staining is interpreted as negative for IRS 0-1, positive with weak expression for IRS 2-3, positive with moderate expression for IRS 4-8, and positive with strong expression for IRS 9-12. In addition, the IRS classification provides further insight, where IRS 0 is considered negative, IRS 1 indicates positive with weak expression, IRS 2 indicates positive with moderate expression, and IRS 3 indicates positive with strong expression. Overall, this analysis provides an in-depth understanding of the presence and intensity of the intended marker in the cells or tissues examined through immunohistochemical staining.
Both in terms of percentage of cell expression and the intensity of the expression of the parameters in question. As a result, the results of the IRS classification also showed better results than the control group (Tables 1 and 2).
Detailed result of histological analysis was detailed on Table 4. From histological analysis, evaluation of tendon healing with Modified Tendon Maturing Score has significant difference in the 2-week activity comparing the control and treatment groups (p<0.05). Histological analysis also found significant difference in number of fibroblasts, blood vessel, and fibrotic tissue (p<0.05) indicating a tangible increase in necessary tissue for tendon healing (Table 4).
The progress in tissue engineering technologies enables the production and analysis of a secretome, which has the ability to stimulate the development of particular tissues like tendons both in laboratory settings (in vitro) and in living organisms (in vivo) [9]. This Secretome is referred to as the tenogenic secretome. Research has demonstrated that the secretome derived from tendons can promote the growth and multiplication of tendon stem cells. Furthermore, it was discovered that the secretome obtained from tendons has a greater ability to sustain its tenogenic phenotype compared to tissue culture plastic alone and matrices derived from bone or skin [10]. Studies have demonstrated that electro-spun aligned Poly L-Lactic Acid (PLLA) fibres enhance the development of spindle-shaped cells, significantly increase the expression of tendon-specific genes (such as collagen type I, collagen type III, collagen type XIV, scleraxis, and elastin), and decrease the expression of osteogenic genes (such as osteocalcin, alkaline phosphatase (ALP), RUNX2), even when exposed to osteogenic media[11].
Several studies have evaluated the regeneration capabilities of the tenogenic secretome, either by itself or in conjunction with a carrier system, in preclinical models including small animals [9-11]. The secretome of mesenchymal stem cells (MSCs) contains various cytokines, chemokines, growth factors, anti-inflammatory factors, and proteins that have potential applications in various diseases. MSCs release TGF-β, a key role in immunomodulation, and produce growth factors like VEGF, HGF-1, and LIF. The galectin network mediates the immunomodulatory effects of MSCs. Extracellular Vesicles (EVs) are a complex communication system that affects recipient cells' functions. They contain 20S proteasome members and regulate cell stability and translation of proteins. MSC-EVs have immunoregulatory and regenerative properties, with miRNAs playing a role in cell cycle regulation and apoptosis [12].
Nevertheless, there is currently a lack of study about preclinical models involving large animals and clinical trial trials. Furthermore, the reparative capacity of pre-treatment tenogenic secretomes has only been evaluated in two trials. The application of Connective Tissue Growth Factor (CTGF) and ascorbic acid to the tenogenic secretome of the rat patellar tendon induces the development of tendon-like tissue in a mouse patella tendon defect model. This is supported by the observed upregulation of tenomodulin, collagen type I, and collagen type III, as well as the downregulation of collagen type II and osteocalcin [13]. Human tenogenic secretomes, when exposed to 5% oxygen tension and applied to Matrigel™, led to the development of adipose, cartilage-like, and bone-like tissues. However, when placed into a matrix produced from tendons, they specifically formed tendon-like tissues in living organisms [14].
TGF-β is an important regulator in tendon healing [7,15-16]. TGF-β affects cell function and gene expression primarily through activation of the Smad signalling pathway. In the context of tendon healing, TGF-β has an important role in collagen synthesis [17]. During the tendon healing phase after an injury, the more elastic collagen type III is initially expressed, and then slowly remodelled into type 1 [18]. The absence of TGF-β interferes with this remodelling process and thus of course collagen type III. As a result, tendons formed under conditions of TGF-β deficiency will have lower tensile strength. Scx has been found to promote attachment between tendon and bone through its important role in tendogenesis which is also important for enthesis repair [19,20-21]. Deficiencies in Scx expression alone can interfere with enthesis development. Specifically, Scx plays a role in inhibiting the formation of osteoclasts by secreting miR-6924-5p-rich exosomes. These exosomes will eventually strengthen the end result of tendon healing [22,23]. Scx as a transcription factor most likely prevents osteoclast formation by regulating the expression of target genes by binding to genetic loci [24]. However, the remaining details of how Scx can affect the inhibition of osteoclast formation are unknown [25]. In addition, Scx is able to affect protein expression from mesenchymal cells and also exosomes which in turn prevents osteoclastogenesis. Collagen type III is essential for fibrillogenesis in tendon tissues, with high levels observed in basic medium and culture medium supplemented with TGF-β. Collagen type III expression decreased by 14 days and increased again by 21 days. Scleraxis, a transcription factor, was upregulated by 7 days in basic and EGF media, especially in TGF-β, and increased in EGF supplemented medium by 14 and 21 days [26]. TGF-β2 treatment significantly upregulated collagen production, cytokines, and growth factors which are relevant to tendon healing [27].
Modified Tendon Maturing Score (MTMS) has an important role in evaluating the regeneration of tendon from histological perspective. This instrument measures the number of cells, the amount of fibrosis, vascularity, parallel cells, and insertions. Healing of tendons is characterized by the formation of scar tissue which can be functional or non-functional. If it is non-functional, the scar tissue can cause tendon injury again at a later time, even causing instability and changes in joint function. Scar tissue deposition usually interferes with the tendon from gliding and moving. This is most visible in tendons covered by a synovial layer, such as in zone II of the hand flexor tendon system. Therefore, we ideally seek for decrease in fibrotic tissues but increase in blood vessel and fibroblast [28].
In this study, it was found that there was an increase in TGF-β, collagen type III, and Scleraxis compared to the control group. Moreover, histologically there is evidence of increase in blood vessel and fibroblast along with decrease in fibrotic tissue. This shows that the administration of tenogenic secretomes is indeed able to induce tendons regeneration indicated by the increased factors that support the regeneration of the tendons. Collagen type III as the progenitor of more mature collagen was also found to increase, indicating that the administration of tenogenic secretomes succeeded in encouraging the collagen formation in damaged tissue in the sample.
Conclusion
The secretome of mesenchymal stem cell (MSCs) contains various cytokines, chemokines, growth factor, anti-inflammatory factors, and protein that have potential as an adjuvant therapy in various diseases. The ability of human tenogenic secretomes to form specific tissues under different condition suggests the potential for future tailored tissue engineering and regenerative medicine approaches for tendon injuries and related conditions.
Acknowledgements
We would like to express our gratitude to the Orthopedic and Traumatology Department of Dr. Soetomo General Academic Hospital (Surabaya, Indonesia) for supporting this study and Cell and Tissue Bank Dr Soetomo General Hospital staff for their kind and dedicated assistance during the preparation of the secretome.
Conflict of Interest
This research has no conflict of interest.
Orcid:
Baskoro Kusumo Riswanto: https://orcid.org/0009-0003-2422-9854
Cery Tarise Hajali: https://orcid.org/0000-0001-5109-2716
Teddy Heri Wardhana*: https://orcid.org/0000-0002-6936-8730
--------------------------------------------------------------------------------------
How to cite this article: Baskoro Kusumo Riswanto, Cery Tarise Hajali, Teddy Heri Wardhana*, The effect of secretome injection on tendon healing of rotator cuff tear on new zealand white rabbit through the expression of tgf-b, scleraxis, collagen type iii, and histological evaluation. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(4), 401-410. Link: http://jmpcr.samipubco.com/article_185692.html
--------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
.png)
