Document Type : Case Report
Authors
1 Clinical Pathology Education Program, Hematology Division, Faculty of Medicine, Airlangga University, Surabaya, Indonesia
2 Clinical Pathology Department, Faculty of Medicine, Airlangga University, Surabaya, Indonesia
3 Anatomical Pathology Laboratory, Dr. Saiful Anwar General Hospital, Malang, Indonesia
4 Clinical Pathology Laboratory, Brawijaya University, Malang, Indonesia
Abstract
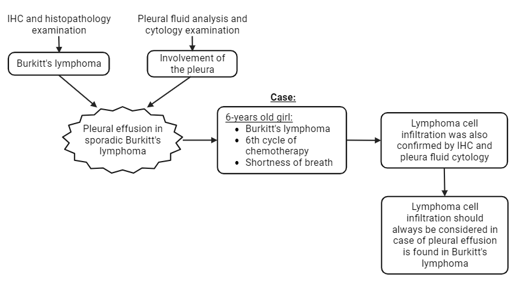
Pleural effusion in sporadic Burkitt's lymphoma is very rare. The diagnosis of Burkitt's lymphoma was confirmed by histopathological and immunohistochemical examination, while pleura involvement was confirmed by pleural fluid analysis and its cytology. We presented a 6-year-old girl diagnosed with Burkitt's lymphoma who came for the sixth cycle of chemotherapy presented with shortness of breath. Lymphoma cell infiltration was confirmed by immunohistochemical examination of the mass in the ileum and pleural fluid cytology. Although rare, the possibility of lymphoma cell infiltration should be considered if a pleural effusion is found in Burkitt's lymphoma.
Graphical Abstract
Keywords
Introduction
Non-Hodgkin lymphoma (NHL) makes up 7–10% of all malignancies in children under the age of 20. Lymphoma is the third most prevalent type of malignancy in children. About 1% to 5% of NHL cases are Burkitt's lymphoma, a B-cell non-Hodgkin's lymphoma [1-4].
Primary pleural malignancies or intrathoracic and extrathoracic malignancies that spread hematogenously, lymphatically, or contiguously to reach the pleural space can cause malignant pleural effusions. Over 75% of malignant pleural effusions are brought on by lymphoma, breast, ovarian, or lung neoplasms [5,6]. Effusion occurs in malignant lymphomas that are highly proliferative, such as Burkitt's lymphoma and lymphoblastic lymphoma, and is linked to a poor prognosis. In this instance, urate-lowering medication may be considered for the patient to diagnose tumor lysis syndrome through examination of the effusion fluid [7]. The purpose of this case report is to discuss malignant pleural effusion in a patient with Burkitt's lymphoma, more importantly its diagnostic management.
Patient and observation
Patient Information
A 6-year-old girl came to our hospital for her last cycle of chemotherapy for Burkitt Lymphoma. The patient also complained of leg pain since the end of the 5th cycle, which was accompanied by swollen feet. The patient had a fever since 3 days prior to the hospital admission. The patient had been diagnosed with Burkitt's Lymphoma of the intestine a year prior, thus subsequently undergoing chemotherapy according to Magrath protocol. At that time, the patient complained of an enlarged abdomen since a month prior, and a mass was identified by MRI. The mass of the ileum was removed by laparotomy, followed by histopathological and immunohistochemical examinations. Immunohistochemical examination showed 100% Ki-67 positive and positive CD20 diffuse pattern suggesting Burkit's lymphoma (Figure 1a and 1b).
Clinical Findings
The patient's vital signs on arrival were within normal limits. Laboratory examination showed Hb 9.8 g/dL, platelets 904,000/uL, and uric acid 7.7 g/dL.
Timeline of current episode
The patient had shortness of breath on the third day, and fluid accumulation was found on physical examination and ultrasound three weeks after her last cycle of chemotherapy.
Diagnostic assessment
Thoracentesis was performed to collect the pleural fluid for analysis. It showed a cloudy yellow fluid with blood clots, the dominantly found leukocytes were mononuclear cells, the pleural fluid total protein was 3.42 g/dL, and the LDH was 11.470 g/dL. On Wright-Giemsa staining, mononuclear cells were found with a basophilic and vacuolated cytoplasmic appearance that matched the Burkitt's lymphoma cells (Figure 2).
Diagnosis
A Burkitt’s lymphoma of the intestine and pleura was confirmed.
Therapeutic interventions
The patient underwent pleural fluid evacuation and received supportive management.
Follow-up and outcomes
The patient returned home on the 12th day of hospitalization with an improved general condition compared to when she was initially admitted. Her last laboratory examination finding showed normal platelets and uric acid levels (platelets 164,000/uL; uric acid 4.2 g/dL) and leukopenia (3,080/uL). The patient was planned for the next chemotherapy a week after her discharge.
Patient Perspective
During her hospitalization, the parents were satisfied with the care she received and seemed optimistic about her status of health. The patient was discharged and planned for the next chemotherapy a week after.
Informed Consent
Written consent was obtained from the patient for publication of this case report.
Discussion
The patient had a history of Burkitt's lymphoma in the ileum which was confirmed with histopathological and immunohistochemical examinations. In the World Health Organization (WHO) classification, Burkitt's lymphoma is defined as a highly aggressive B-cell neoplasm that often presents extranodally or as an acute leukemia [8]. Macroscopically, gastrointestinal involvement presents as a large mass with bowel wall thickening and hemorrhage, often associated with multiple polypoid lesions. Histologically, the lymph node structure eventually disappears and a characteristic diffuse proliferation can be found, with a clear starry-sky pattern seen in small visual fields [9,10]. Burkitt lymphoma is also characterized by a c-myc translocation, CD10+/bcl-2-/bcl -6+ with a very high Ki-67 proliferation index, and positive B cell antigens such as CD19, CD20, CD22, and CD79a [11,12].
Based on the geographical distribution, Burkitt's lymphoma have 3 types, which are endemic (eBL) found in Africa, sporadic (sBL) found in countries other than the African continent, including Europe and Asia, and the last is associated with immunodeficiency (iBL). Our patient can be classified as sporadic type, because the patient is Asian. The majority of the sporadic type occurs in children and involves the abdominal organs, especially the ileocecal, up to about 80% of cases [9].
Pleural effusion was present three weeks after her completion of fifth cycle of chemotherapy [13]. Pleural effusion is an accumulation of fluid in the pleural space which is classified as transudate or exudate according to its composition and underlying pathophysiology [14,15]. Pleural effusion in patients with low immune status can be associated with non-malignant processes, such as infection. However, it can also be associated with malignancies, such as sarcoma. Kaposi's, thoracic non-Hodgkin's lymphoma, or primary effusional lymphoma [16]. Malignant pleural effusion diagnosis is made when malignant cells in the pleural fluid was found. It is a pathological process that indicates a failure of defense mechanisms in the pleura and mesothelial function. Malignant pleural effusion is naturally an exudate characterized by high protein and lactate dehydrogenase (LDH) on pleural fluid analysis [17-19].
The patient was discharged with a complete blood count showing leukopenia. The pediatric patient with Burkitt's lymphoma at Dr. Saiful Anwar General Hospital underwent chemotherapy according to Magrath protocol. In the last cycle of chemotherapy, the patient received high-dose methotrexate and leucovorin. Methotrexate is a chemotherapeutic agent that stops DNA anti-metabolites so that it has a risk of myelosuppression, causing neutropenia and megaloblastic anemia. However, this can be managed by administering leucovorin-a folic acid supplementation [20]. In this patient, there may be a marrow suppression after the third day of treatment, but has shown improvement until the 12th day.
Conclusion
Burkitt’s lymphoma is a very aggressive tumor with varied manifestations. In children with sporadic Burkitt's lymphoma, the majority of cases involve the abdominal organs, particularly the ileocecal. The manifestation of pleural effusion is rare. Therefore, in Burkitt's lymphoma patients who complain of shortness of breath, the possibility of pleural effusion should be suspected. It is necessary to undergo radiology examination to confirm the presence of pleural effusion, and perform pleural fluid analysis and cytology to determine the cause. Burkitt's lymphoma in children has a decent possibility of recovery if intensive chemotherapy is immediately performed.
Acknowledgments
The authors would like to thank the patient and the support of the staff in hematological and all other lab studies.
Conflict of interest
The authors have no conflict of interest regarding this investigation.
Authors’ contributions
The case report was written by Dian Sukma Hanggara, the figures of immunohistochemical examination was interpreted and assured by Hendy Setyo Yudhanto, the figures of cytology analysis was interpreted and assured by Edwin Darmawan, and the review by Paulus Budiano Notopuro. All the authors have read and agreed to the final manuscript.
Orcid:
Dian Sukma Hanggara*: https://orcid.org/0000-0002-0881-096X
Paulus Budiono Notopuro: https://orcid.org/0000-0001-6927-2205
Hendy Setyo Yudhanto: https://orcid.org/0009-0006-2713-8247
Edwin Darmawan: https://orcid.org/0000-0001-8315-7166
----------------------------------------------------------------------------------
How to cite this article: Dian Sukma Hanggara* ,Paulus Budiono Notopuro, Hendy Setyo Yudhanto, Edwin Darmawan, Pleural efusion in burkitt’s lymphoma: a case report. . Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(4), 411-416. Link: http://jmpcr.samipubco.com/article_185736.html
----------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
