Document Type : Original Research Article
Authors
Child Health Department of Dr. Soetomo General Academic Hospital, Faculty of Medicine, Surabaya, Indonesia
Abstract
Pneumonia is a significant contributor to global child mortality, accounting for approximately 15% of total deaths in children under five. Vitamin D deficiency has been identified as a potential factor in respiratory tract infections. This study aimed to investigate the impact of vitamin D3 on calcidiol, IL-10, and pneumonia severity in children, offering valuable insights into the relationship between vitamin D3 supplementation, IL-10 levels, and pneumonia severity. Conducted on children aged 1 month to 5 years diagnosed with pneumonia, the research employed a rigorous experimental design, including double-blind procedures, a control group, pretest-posttest measurements, and appropriate controls. Data collection took place from March to June 2022. Participants received standard therapy and a single oral dose of 100,000 IU of vitamin D3 (cholecalciferol). Calcidiol and IL-10 levels were assessed, with serum levels examined after 8 days. Statistical analyses using Mann-Whitney U test and paired t-test in SPSS version 25 were conducted. The study comprised 46 participants (30 males, 16 females) with an average age of 24 months in the control group. Post-supplementation, calcidiol levels were 53.08 ± 64.5 ng/mL (p = 0.04), while IL-10 levels were 130.39 pg/ml (p=0.27). A significant difference in pneumonia severity was noted post-supplementation compared to the pre-supplementation period (p<0.001). Thus, vitamin D3 supplementation influenced pneumonia severity, but did not significantly impact IL-10 level changes. This study sheds light on potential avenues for improving pneumonia outcomes in children through targeted vitamin D supplementation.
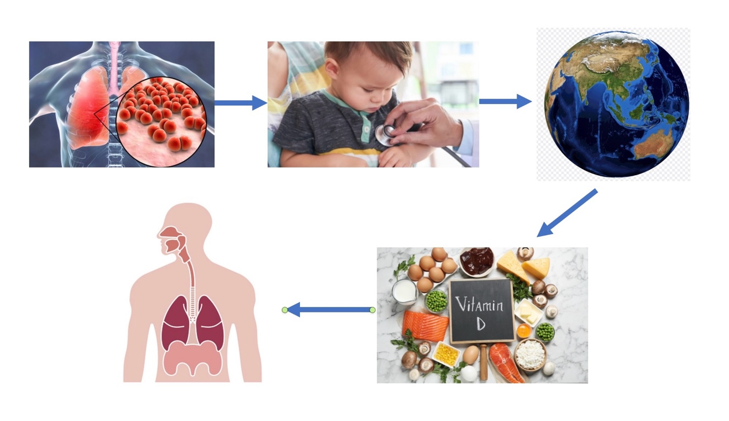
Graphical Abstract
Keywords
Introduction
Pneumonia remains a significant respiratory infection, contributing to 29% of global child mortality among children under the age of five [1]. As per the analysis of certain specialists, there exists a potential association between insufficient levels of vitamin D and an increased susceptibility to respiratory tract infections among youngsters. This correlation may result in a notable elevation in the risk of pneumonia, namely among children below the age of five, by a factor of thirteen. Moreover, there exists a correlation between inadequate levels of vitamin D and the severity of illness, duration of therapy, as well as complications associated with pneumonia [2-5]. Vitamin D has been shown to enhance the activity of macrophages and dendritic cells, leading to immunomodulatory effects. This is achieved by the reduction of pro-inflammatory cytokines and the enhancement of anti-inflammatory cytokines [6]. Interleukin-10 (IL-10) is a cytokine with anti-inflammatory properties, being secreted in response to inflammatory stimuli within the body. It plays a pivotal role in immune system modulation and the attenuation of inflammatory processes [6-8]. This cytokine is influenced by vitamin D levels and known as key role in controlling excessive pro-inflammatory cytokine responses [6-10].
There are 90% of pneumonia cases in developing countries. In Indonesia, pneumonia is the leading cause of child mortality in the age group of 29 days to 11 months due to infection, with 979 deaths, and is the second leading cause of death after diarrhea in the age group of 12 to 59 months. The World Health Organization (WHO)'s disease management strategies have significantly reduced the incidence of pneumonia, although child mortality remains high [5]. Based on a meta-analysis conducted, it was shown that children diagnosed with community-acquired pneumonia (CAP) and exhibiting a deficit in vitamin D (with a serum 25(OH)D level of 20 ng/ml) were observed to have a notably higher likelihood of developing pneumonia (odds ratio (OR) = 1.64, 95% confidence interval (CI): 1.00; 2.67) [11].
According to the study conducted by Jingi et al. (2018), it was suggested that the administration of vitamin D supplements to children below the age of five who have been diagnosed with pneumonia and severe pneumonia resulted in a significant decrease in the likelihood of recurrence within a three-month period [12]. However, a study with different results was conducted by Manaseki-Holland et al. (2017), which vitamin D3 supplementation in infants, resulted were not significant in the treated control group [13]. A study of 34 children with pneumonia found significantly decreased serum IL-10 levels in severe pneumonia compared to mild pneumonia (P<0.01) [6]. Vitamin D levels are associated with increased IL-10 production through B lymphocytes, and increased IL-10 output has been associated with prognosis improved and shorter recovery in children with pneumonia, although data are still limited [14,15].
In the instance of pediatric pneumonia, the effects of vitamin D administration as an immunomodulator on IL-10 levels should be investigated further. This study aims to analyze the effect of vitamin D3 supplementation on calcidiol levels, IL-10, and the severity of children with pneumonia. This work holds considerable significance in enhancing the comprehension of the impact of vitamin D3 supplementation on IL-10 levels and the severity of pneumonia in pediatric patients. The findings of this study may shed more light on the potential significance of vitamin D3 as a determining factor in reducing the symptoms and impact of childhood pneumonia. By better understanding, more effective management strategies can be developed to improve the health and quality of life of children who are vulnerable to this disease.
Materials and methods
Study design
The present investigation utilized an experimental methodology, incorporating a pretest-posttest control group design and double-blind protocols. The study focused on a sample of children ranging from 1 month to 5 years of age who were diagnosed with pneumonia at RSUD Dr. Soetomo Surabaya.
The data collection period spanned from March to May 2022. The study population comprises individuals who satisfied the predetermined criteria for inclusion and exclusion, along with the establishment of specific criteria for discontinuation of participation in cases of specified conditions. Inclusion criteria included children aged one month to five years, diagnosed with pneumonia, and who had received permission from their families after signing informed consent. Participants who had received vitamin D3 supplements within four weeks prior to the study, participants who had undergone antibiotic therapy for more than three days prior to the study, and participants with renal failure, a history of congenital heart
disease, acute post-Streptococcus glomerulonephritis, or a history of allergy to vitamin D3 were all excluded from the study. Discontinuation of the study may occur if the patient develops complications related to calcium metabolism during the study process, the parents withdraw, or the study subject dies.
Data collection
The participants in the supplementation group were administered a solitary dose of 100,000 IU of vitamin D3 (cholecalciferol) orally or via nasogastric tube, whereas the control group got a placebo. Both groups received standard antibiotic therapy for pneumonia. The sample size was 17 children each group. After estimating the anticipated rupture of 25% Higgins correction, the sample size of each group was set to 23. The first visit was conducted at the time diagnosis of pneumonia and involved history taking physical examination, and blood tests. The second visit was conducted seven days after the first visit and the evaluation of the study sample included history taking, physical examination, and blood tests. The calcidiol level is defined as the measurement of the serum level of calcidiol (25-OH hydroxyvitamin D3) using the enzyme-linked immunosorbent assay (ELISA) technique. Vitamin D levels are typically classified into three distinct categories: normal (ranging from 30 to 100 ng/mL), insufficiency (ranging from 21 to 29 ng/mL), and deficiency (below 21 ng/mL). Concurrently, the levels of IL-10 in the peripheral blood were assessed through the utilization of the Enzyme-Linked Immunosorbent Assay (ELISA) technique, with the results being quantified and reported in picograms per milliliter (pg/ml). Pneumonia severity was measured using the pediatric Respiratory Severity Score (PRESS) system with components included respiratory rate, presence of wheezing, respiratory muscle use, blood oxygen saturation, and difficulty drinking or eating. Data are given on an ordinal scale. The classification of PRESS scores is specified in Table 1.
Statistics
The research findings were reported as median, ratio, and raw (SD) comparisons. The normality of the data was assessed using the Kolmogorov-Smirnov test. The descriptive statistics of this study encompassed measures such as frequency (n), median, mean, and percentage (%). The correlation of calcidiol levels with IL-10 levels and severity was done with the Spearman test. Comparison before and after vitamin D3 administration was done with the Wilcoxon test. In addition, comparisons between calcidiol, IL-10, and gravity levels in both groups used the Mann-Whitney test.
Ethical clearance
This research was registered in the research ethics issued by the Health Research Ethics Committee of Dr. Soetomo General Academic Hospital, Surabaya, under number 0379/KEPK/III/2022.
Results
Characteristics of subject patients
The median age in the supplementation group was 24 (3-60) months, while the control group had a median age of 10 (2-60) months. In addition, the proportion of female gender was equal to the number of males in each group. The nutritional status of the subjects in this study was mostly good nutrition, with a percentage of 56.6% in the supplementation group and 65.4% in the control group. There were 26.1% of subjects who were malnourished in each group (Table 2). We evaluated the correlation of calcidiol level with the severity of pneumonia at the first evaluation from all samples (both groups). According to the analytic assessment, we found that there was no significant correlation between the calcidiol level (p = 0.666) and IL-10 level (p = 0.969) with pneumonia severity in child. (Table 3).
Calcidiol measurement results after supplementation
Calcidiol levels in the group experienced significant changes before and after supplementation. At the end of the study, the median calcidiol level in the supplementation group reached 53.08±64.5) pg after supplementation (Table 4).
Results of measurement of IL-10 levels after supplementation
IL-10 levels in the group did not show significant changes before and after supplementation. At the end of the study, the median IL-10 level in the supplementation group reached 130.39 (44.08-1109.78) pg after supplementation (Table 5).
PRESS score after supplementation
The severity of pneumonia, based on the PRESS score in the pre- and post-supplementation groups, showed increased after vitamin D3 supplementation (Table 6).
Discussion
The objective of this study was to evaluate the effectiveness of a solitary dose of 100,000 IU vitamin D3 provided orally or through a nasogastric tube in mitigating pneumonia outcomes in pediatric patients, while concurrently exploring the mechanism underlying the anti-inflammatory cytokine response. The PRESS score was used to identify patients in this study depending on the severity of their pneumonia, namely mild, moderate, and severe. PRESS scores in both groups were largely similar in both the control and supplementation groups, with approximately 89.1% of subjects having severe PRESS scores and 10.9% categorized as moderate. The clinical manifestations of pneumonia are indicative of the extent of the respiratory ailment, and these diagnostic observations hold significance in promptly identifying the condition and administering suitable therapeutic measures. Therefore, proper treatment of acute respiratory infections is crucial in preventing the risk of respiratory failure. Serious cases should be treated quickly, as assessment of the respiratory condition should be done promptly at first contact. Heart rate and blood pressure assessment is not included in the PRESS score due to the challenges associated with evaluating these measures in weeping children. In addition, the world Health Organization (WHO) states that most healthy children can fight infections with their natural defenses. Children with impaired immune systems have a higher risk of developing pneumonia. Illness and environmental factors can also increase a child's susceptibility to pneumonia [16].
In the first stage of our analysis, we examined the relationship between calcidiol (p = 0.666) and IL-10 levels in all participants, as well as their association with the pneumonia severity. However, our findings did not reveal a statistically significant link between these variables. Besides the Cairo study, a research inquiry was conducted to assess the vitamin D levels in children aged six months to three years who had pneumonia. The participants were classified into two distinct groups: the vitamin D group and the group including healthy children. The results indicated that there was no statistically significant disparity in vitamin D levels between the two groups (p=0.48) [17]. Based on a study conducted in Indonesia, it was observed that there was a notable prevalence of vitamin D deficiency among children who were sent to the hospital for pneumonia. However, no link was found between vitamin D insufficiency and pneumonia [18]. Meanwhile, another study in Jakarta noted that 60.8% of patients showed normal vitamin D status, 37.5% were in insufficiency status, and 1.7% of patients with vitamin D deficiency status. The study also found that the duration of sun exposure was significantly the main influential factor (p = 0.004) [19]. There was no observed correlation between IL-10 levels and the pneumonia severity across all samples, as determined by IL-10 levels. The present discovery diverged from a previous investigation involving 34 children diagnosed with pneumonia, wherein a notable decline in serum IL-10 levels was observed in cases of severe pneumonia as opposed to mild pneumonia (P<0.01). A study of children with mycoplasma pneumonia also showed significantly decreased serum IL-10 levels in severe pneumonia compared to mild pneumonia. In children with pneumonia, increased IL-10 production is associated with a better prognosis and shorter recovery [14].
The present investigation demonstrated a statistically significant elevation in calcidiol levels subsequent to the administration of a single dose of 100,000 IU of vitamin D3 (p=0.04). However, there was no statistically significant alteration observed in IL-10 levels (p=0.274), which deviates from the existing body of literature. Prior research has demonstrated that vitamin D exerts an influence on the immune system by inhibiting the proliferation of T cells, restricting the production of pro-inflammatory cytokines like INF, and governing the transcription of the IL-10 gene, resulting in elevated levels of IL-10 [9,20,21]. Experimental research results showed that 1,25-OH vitamin D can enhance Th2 and Treg cells while inhibiting Th1 and Th17 cells [22]. On the other hand, increased IL-10 levels may occur through prohibition of dendritic cell proliferation and maturation [23].
This study used a different dose and duration of Vitamin D3 supplementation than earlier studies. Despite observing a higher increase in IL-10 levels in the vitamin D group (7.7 compared to 5.9 in the placebo group), no statistically significant difference was found between the two groups. Following the administration of supplements, it was seen that 23 out of 25 individuals in the vitamin D group exhibited interleukin-10 (IL-10) levels exceeding 9 pg/ml. In comparison, 24 out of 27 participants in the placebo group displayed IL-10 levels over the aforementioned threshold. The odds ratio for this comparison was calculated to be 1.44 (95% confidence interval [0.22, 9.41], p=0.70). Besides the use of Vitamin D supplements, the initial use of antibiotics and the subsequent improvement in the clinical condition of the patient may also result in fluctuations in the levels of IL-10. Vitamin D has been observed to enhance the production of IL-10 while concurrently inhibiting the transcription of IgE through B lymphocyte cells. The activation of the vitamin D receptor (VDR) and cytochrome P450 1a (CYP1a) induces the synthesis of calcitriol by B cells. By boosting IL-10 expression in response to calcitriol signaling and reducing epsilon-germline transcription, this process is maintained [9].
IL-10 levels may vary in children with pneumonia, and the specific changes may depend on the type and severity of the infection. Another possible theory for Vitamin D's role in reducing pneumonia severity other than the anti-inflammatory cytokine enhancement pathway is a decrease in proinflammatory cytokine levels or an increase in antimicrobial peptide levels. The metabolite 1,25(OH)2D, which is an active form of Vitamin D, has been observed to decrease the expression of toll-like receptors on monocytes and also hinder the synthesis of inflammatory cytokines like IL-2, IL-6, and IL-17 [2]. The active metabolite 1,25(OH)2D also enhances the antimicrobial activity of macrophages and monocytes by autocrine signaling via the VDR-RXR pathway, leading to the production of the endogenous antimicrobial peptide cathelicidin LL-37 [2,24].
A disparity in the degree of severity was observed between the control and treatment groups in the conducted research, whereby a singular dosage of 100,000 IU of vitamin D3 supplementation was administered. Based on the PRESS score, there was a difference in the severity of pneumonia following supplementation in the control and supplementation groups (p=0.004). Furthermore, changes in PRESS scores after supplementation in both groups were analyzed. In the control group, some subjects did not experience an increase in PRESS scores, while in the supplementation group, all subjects experienced a decrease in PRESS scores. The PRESS score is used to perform a rapid assessment of the condition of a child's respiratory infection in distress [25].
A previous study in India, using a systematic review scheme, compared therapy with vitamin D and placebo in pediatric pneumonia patients aged <5 years. There was no statistically significant difference observed between the two groups with regard to variables such as hospitalization duration, hospital release completion time, chest discomfort, or drinking concerns. The Cochrane review examined four trials encompassing a total of 780 children diagnosed with pneumonia, as well as three studies containing 749 children diagnosed with severe and very severe pneumonia. Notably, all participants in these trials and studies were under the age of five. Vitamin D supplementation was done in a variety of ways and doses. However, the quality of the evidence used was weak, so the reviewers were not convinced that oral vitamin D administration as an adjunctive therapy for pneumonia could affect the external effects of pneumonia [26]. Extensive investigation has been conducted on the association between vitamin D and various ailments, including infectious diseases, yielding positive results. Based on specific research findings, it has been shown that vitamin D may have a potential beneficial effect in the management of pneumonia. A study conducted at Cairo Teaching Hospital employed a randomized, double-blind, placebo-controlled design to investigate the effects of vitamin D3 supplementation. The findings revealed that the administration of vitamin D3 resulted in a reduction in mortality risk and the Pediatric Sequential Organ Failure Assessment (pSOFA) score. In addition, it was seen that the supplementation led to a shortened recovery period and an improvement in the PaO2/FiO2 ratio [27]. The disadvantage of this study is that it did not account for a variety of cytokines at each stage of vitamin D's activity, so it does not explain how the dominance of vitamin D in its role can reduce the severity of pneumonia. In this study, screening calcidiol levels and vitamin D supplementation seem to provide promising benefits on pneumonia outcomes, which are expected to be continued in further studies.
Conclusion
The levels of calcidiol and IL-10 showed no correlation with the severity of pneumonia in children with the disease. Despite observing a notable rise in calcidiol (25[OH]D) concentrations, there was no concurrent elevation in IL-10 levels among the participants who were administered vitamin D3 supplementation. Further multi-center studies are needed to gain more comprehensive understanding the effect of vitamin D on the severity of pneumonia in children.
Acknowledgements
None.
Orcid:
Yana Fina Yusriy: https://www.orcid.org/0009-0007-8332-4615
Setyoningrum Retno Asih: https://www.orcid.org/0000-0002-4194-6869
Irawan Roedi: https://www.orcid.org/0000-0001-5999-4773
---------------------------------------------------------------------------------------
How to cite this article: Yana Fina Yusriy, Setyoningrum Retno Asih*, Irawan Roedi, Effect of vitamin D3 supplementation on Il-10 level and severity of pneumonia in children: a randomized double-blind placebo-controlled trial. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(4), 417-427. Link: http://jmpcr.samipubco.com/article_185745.html
---------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
.png)
.png)
