Document Type : Original Research Article
Authors
- Yeganeh Youzbashizadeh 1
- Morteza Saeedi 2
- Zahra Abbasi Shayeh 3
- Ehsan Bolvardi 4
- Maryam Sobhani 5
- Mahdi Foroughian 4
- Maryam Ziyaei 6
- Fatemeh Maleki 7
- Amir Masoud Hashemian 4
1 Department of Emergency Medicine, Mashhad University of Medical sciences, Mashhad, Iran
2 Department of of Neurology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
3 Department of of Community Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
4 Department of Emergency Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
5 Department of of Emergency Medicine, North Khorasan University of medical sciences, Bojnurd, Iran
6 Department of Emergency Medicine, Faculty of Medicine,Zahedan University of Medical Sciences, Zahedan, Iran
7 Department of Emergency Medicine, Faculty of Medicine, Birjand University of Medical Sciences, , Birjand, Iran
Abstract
Background and aim: Assessment of the prognosis of the intracranial hemorrhage (ICH) is important in case of patients’ follow up and management. It is reported that there might be some links between serum troponin levels (TPI) and ICH. However, there is a gap of knowledge in case of nontraumatic cases. The aim of this study was to investigate the relationship between TPI and prognosis of patients with non-traumatic cerebral hemorrhage.
Method: This retrospective cohort study was conducted on all non-traumatic stroke patients referred to the emergency room of Ghaem Hospital (AJ) on patients with confirmed ICH in CT scan. Patients were included in the study after obtaining consent from them or their legal guardians. Brain CT scan was used to determine the location and volume of bleeding, midline changes, and presence of intraventricular hemorrhage (IVH). The bleeding volume was estimated using the formula (ABC)/2. The primary troponin (cTnT) test was performed within 12 hours of the onset of symptoms for each patient. A serum cTnT value ≥0.01 ng/ml was set as the cut-off value, and then the patients were divided into two groups: normal troponin and increased troponin level, and also their prognosis was determined based on the ICH Score and Predicting Mortality after Acute ICH table. Next, after 3 days, all patients in both groups were contacted and their disease status was determined based on the Modified Ranking Scale. The collected data were subjected to statistical analysis by SPSS.
Results: A total of 387 patients were included in our study, including 214 men (55.3%) and 173 (44.7%) women. The average age of the patients was 66.16 years and ranged from 19 to 95 years. 81 patients (20.9%) had increased troponin based on the determined level. In addition, 174 patients (45.0%) died during hospitalization. The mean of ICH Score was 2.37 ± 0.99 and the mean of Modified Ranking Scale was 3.24 ± 2.49. There was no significant difference in terms of troponin level (p=0.250) and gender (p=0.508) between those who died and those who were discharged with partial recovery.
Conclusion: There was no significant relationship between troponin and the outcome of non-traumatic brain hemorrhage patients, but after adjustments, the troponin levels were increased. However, it seems that the level of 0.01 ng investigated in our study is not suitable, and it is possible that other levels will provide better results.
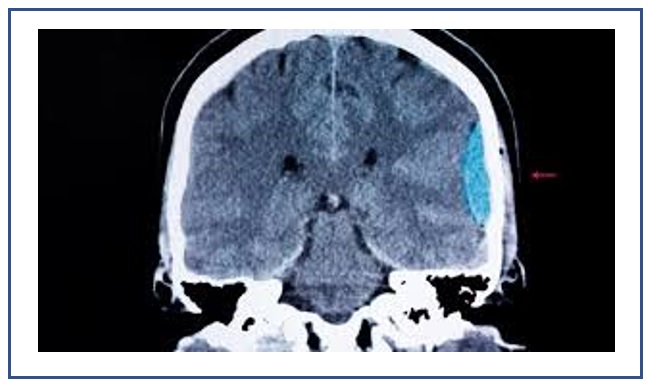
Graphical Abstract
Keywords
Main Subjects
Introduction
Nontraumatic brain injury (NTBI) is defined as the brain damage caused by pathologies other than trauma including infection, cerebrovascular disease, neoplasm, poisoning/neurotoxicity, and autoimmune disorders [1-2].
The main underlying pathophysiology in the damage caused by NTBI is ischemia and hypoxia/anoxia. The NTBI epidemiology differs according to the related etiologies. Stroke is the most common cause of NTBI in adult population, while infection is the most common etiology in pediatric population [3-4].
The NTBI epidemiology differs according to its etiology. Annually 1.2 million cases develop meningitis and 1.4 million patients develop encephalitis. Moreover, the annual incidence of stroke is 30 to 120 per 100000 [5].
Furthermore, NTBI constitutes a high burden on patients, their caregivers, and the society. The damage spectrum can predict the amount of disability that is posed to the patient. This disability can affect the patients’ quality of life. Besides impairments, NTBI causes considerable mortality. According to the NTBI etiology, the mortality ranges between 3 to 84 percent among different societies [6-7].
The mater of patients’ stratification according to their prognosis is important, with this regard. Previously it was reported that patients with critically ill condition have elevated levels of troponin (TnI) [8].
Some believes that patients diagnosed with acute stroke or subarachnoid hemorrhage demonstrates elevated TnI, as a consequence of cardiac injury. However, it is reported that this elevation may happen regardless of the presence of coronary diseases. Although the prognostic role of TnI marker has been widely investigated in traumatic brain injury, few studies have addressed its prognostic role in NTBI [9-11].
This study investigated the role of TnI in NTBI patients’ prognosis.
Material and methods
Study sample and design
This retrospective cohort study was conducted on a sample of NTBI cases who referred to emergency room of Ghaem Hospital. The included patient should have confirmed diagnosis of intracranial hemorrhage and patients or their legal guardians should be provided with written informed consent. To calculate the sample size, troponin along with five predictors of mortality was enrolled in the regression model. It was assumed that 15 cases per variable were needed and according to the presence of four variable 60 cases were enrolled. Moreover, the 3 days prevalence of mortality was assumed as 25% and with this regard 340 cases should be assessed. Finally, given that a 10 percent lost to follow up, the final sample size was calculated as 270 patients.
Data collection methods
All the patients underwent CT scan, to assess the location and volume of bleeding, midline shift, and intraventricular hemorrhage. The volume of hemorrhage was assessed using (ABC)/2 formula. The cardiac troponin (TnI) was assessed during the first twelve hour after the symptom presentation. According to the cut off of 0.01 ng/ml, the patients were classified into two groups including elevated TnI (TnI≥0.01 ng/ml) and normal TnI (TnI<0.01 ng/ml).
Moreover, intracranial hemorrhage predicting Mortality after acute intracranial hemorrhage (ICH) score and Modified Ranking Scale (MRS) were assessed for all patients. The study data were compared according to the level of troponin and patients’ outcomes. The study’s primary outcome was in-hospital mortality. The secondary outcomes were ICH score and MRS.
Ethics
All the patients or their legal guardians were provided with written informed consent and they were free to leave the study whenever, they wanted. Moreover, all the extracted data were recorded anonymously and coded to be kept as top secret. Also, all the steps of this study were according to the Helsinki’s declaration and was confirmed by Ethics Committee of Mashhad University of Medical Sciences (Ethic code: IR.MUMS.MEDICAL.REC.1398.465).
Statistical analysis
The data were entered in SPSS software version 20 for further analysis. Frequency and percent of the qualitative data and mean, standard deviation, median, and interquartile range of the quantitative data were calculated. Gender and troponin status was compared between those with normal TnI and elevated TnI, using chi-square test.
Furthermore, MRS and ICH score compared according to the outcome of the patients. Finally, univariate linear regression analysis conducted using age, gender, MRS score, ICH score, and troponin level, as variables. P-values less than 0.05 considered significant.
Results
Totally 387 confirmed NTBI patients including 214 males (55.3%) and 173 females (44.7%) were enrolled in the study. The mean age of the studied cases was 66.16 years old and ranged between 19 to 95 years old. Table 1 presents demographic data, ICH and MRS scoring results, troponin level status, and discharge status.
Table 1 also compares age, gender and troponin level according to the follow up status. There was no significant
difference regarding gender (p=0.508) and troponin status (p=0.250) between patients who survived the condition and those who succumbed. But dead participants had significantly higher ages than recovered ones (P=0.034).
Furthermore, the mean values of ICH score was significantly higher in dead persons than survived participants (P<0.001). There was also no significant difference regarding ICH score (p=0.653) and MRS score (p=0.250) between normal and elevated troponin status, as well as the age (P=0.356) and gender (P=0.414).
 The length of hospitalization was not different based on death and troponin status (P>0.05).
The length of hospitalization was not different based on death and troponin status (P>0.05).
As indicated in Table 2, the correlation between troponin level and the other variables is generally weak. Troponin level shows a minor positive correlation with age (r = 0.051), a minor negative correlation with length (r = -0.047), and negligible correlations with ICH (r = -0.009) and MRS (r = -0.028), although none of these correlations were statistically significant (all p > 0.05).

Age showed a statistically significant positive correlation with ICH (r = 0.277, p < 0.01) and MRS scores (r = 0.137, p < 0.01), indicating that older individuals are more likely to have higher ICH severity and worse functional outcomes. Length of hospitalization shows no significant correlations with other variables. ICH demonstrates a significant positive correlation with age (r = 0.277, p < 0.01) and a strong positive correlation with MRS scores (r = 0.431, p < 0.01), indicating that as ICH severity increases, both age and functional impairment tend to rise. MRS scores showed a statistically significant positive correlation with age (r = 0.137, p < 0.01) and a strong positive correlation with ICH (r = 0.431, p < 0.01).
55.0% of the 387 total cases experienced mortality, with negative troponin status (tropstatus 0) accounting for 56.7%, and positive troponin status (tropstatus 1) for 48.8% of deaths. Mean survival times for negative and positive troponin status were 45.786 and 30.283, respectively, with corresponding median survival times of 27.000 and 24.000. Overall comparisons utilizing the Log Rank test (Mantel-Cox) (P=0.585), indicated no statistically significant difference in survival distributions between troponin status categories (Figure 1).

FIGURE 1 Probability of survival over time for different groups of troponin positive and negative patients
Discussion
There was no significant relationship between troponin level status and ICH patients’ 3-days prognosis. Furthermore, there was no significant difference regarding the outcome between the two different statuses of the patients. Moreover, no relationship was found between troponin serum level and MRS score. Similar, to out finding Gupte et al. (10) proposed that there was no relationship between TnI and ICH patients’ prognosis in an adjusted multivariate regression model. However, they used the cut-off of more than 0.5 ng/mL, for the classification.
However, there were several studies that proposed a relationship between troponin level and NTBI cases’ prognosis. Tanabe et al. [9].
categorized subarachnoid hemorrhage (SAH) patient, according to the TnI into three groups including negative (TnI<0.1 ng/ml), mildly positive (0.1-1 ng/ml), and highly positive (TnI>1.0 ng/ml). The results showed that Hunt-Hess grade of SAH was higher in patients with highly positive TnI compared to the mildly positive and negative TnI cases; however, there was no significant difference between negative and mildly positive patients in case of Hunt-Hess grade. However, this study was limited with its retrospective manner. Moreover, the cut offs that were used were different from our study.
Naidech et al. [12].
also tried to assess the prognostic role of TnI in SAH patients. They reported that significant elevation of TnI after SAH was associated with an increased risk of cardiopulmonary complications, delayed cerebral ischemia, and death or poor functional outcome at discharge. However, unlike our study that assessed only 3 days outcome of the patients, they assessed the three-month outcome. Sandhu et al. [13].
assessed the role of the cut off of 0.4 ng/ml for the categorization of patients into normal TnI and elevated TnI. They reported the rate of in-hospital mortality, as 64 percent in elevated TnI group and 28% in normal TnI group, which was significantly higher in elevated TnI group. There was two differences between the method of our study and Sandhu et al. work, we used the cut-off of 0.01 ng/ml. Another study conducted by Ramappa et al. [14].
considered TnI levels higher than 2 ng/ml, as elevated levels. They also reported a significantly higher rate of mortality in those with elevated levels of TnI, as patients with normal TnI had a mortality rate of 27% and those with abnormal TnI levels had a mortality of 55%.
Different studies are conducted, but all suffered from limitations due to different facts. One important point is the variety in the use of the cut-off for abnormal TnI level. Moreover, different studies used different prognosis timing, some were confined to the in-hospital outcome and the other was about 3-months prognosis. Maybe, there should be studies in case of long term and short-term prognosis and our study tried to cover this fact to some extent. The final point is the retrospective manner of all above- mentioned studies. We tried to full fill this shortcoming, as our study was longitudinal research.
Recently, Guette et al. [11] also conducted a recent study to define a prognostic cut-off for TnI. They tried to assess the 3-months outcome of ICH patients. They proposed that the level of TnI is related with the severity of ICH according to the MRS. The best proposed cut-off in their study was 22 ng/ml with a sensitivity of 71% and specificity of 58%. It is believed that the elevation in serum TnI is a result of cardiac dysfunction that occurred after NTBI. It is reported that ECG abnormalities is a frequent finding that may be found in even more than half of the cases [15-17].
Among biochemical markers, TnI is a more sensitive marker of myocardial injury than Creatine kinase MB fraction (CK–MB), which is consistent with the cardiac literature. Accordingly, this added to the popularity of TnI for prognosis stratification (16, 18-20). However, it should be investigated the prognostic role of the TnI is related to cardiac dysfunction or not and what extend of dysfunction should be noted, as important. It may be possible that low levels of injury, as are documented with low TnI levels has no prognostic value.
As a limitation, Troponin is a nonspecific biomarker, so we conducted a rigorous statistical analysis adjusting for key covariates, including age, gender, and ICH score. This multivariate approach is designed to control for potential confounding factors and isolate the specific impact of troponin on mortality risk. But other events like autonomic nervous system regulations, ICH effect on hemodynamic instability, systemic inflammatory responses, can affect the troponin levels in body and the cardiac function is not evaluated in this study.
Conclusion
This study demonstrated that TnI, using the level of 0.01 ng/ml, cannot have a prognostic role in NTBI patients. Still, the other serum levels may present prognostic values. We studied the prognosis of our cases within a period of 3 days. However, it can be advised for other researchers to use different cut-offs and assess both short term and long-term outcome of the patients. In case of quantitative measurement of TnI, receiver operator curve design can find a real prognostic level. Further studies are needed to make a conclusion regarding the prognostic value of the TnI in NTBI cases.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Ghaem Educational and Research and Therapeutic Center of Mashhad University of Medical Sciences for providing facilities to this work.
Funding
This study was supported by Mashhad University of Medical Sciences.
Authors' Contributions
All authors contributed toward data analysis, drafting, and revising the manuscript and agreed to be responsible for all the aspects of this work.
ORCID:
Morteza Saeedi: https://www.orcid.org/0000-0002-9222-3660
Ehsan Bolvardi: https://www.orcid.org/0000-0003-0255-1861
Maryam Sobhani: https://www.orcid.org/0000-0001-8621-3186
Mahdi Foroughian: https://www.orcid.org/0000-0002-3944-9361
Maryam Ziyaei: https://www.orcid.org/0000-0003-1693-6818
Fatemeh Maleki: https://orcid.org/0000-0002-6823-5151
Amir Masoud Hashemian*: https://orcid.org/0000-0001-5668-6599
-----------------------------------------------------------------------
How to cite this article: Yeganeh Youzabashizadeh, Morteza Saeedi, Zahra Abbasi Shayeh, Ehsan Bolvardi, Maryam Sobhani, Mahdi Foroughian, Maryam Ziyaei, Fatemeh Maleki, Amir Masoud Hashemian*, Serum troponin level relationship with prognosis of nontraumatic cerebral hemorrhage. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(4), 447-455. Link: http://jmpcr.samipubco.com/article_186086.html
-----------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.