Document Type : Original Research Article
Authors
KIIT School of Management, KIIT University, Bhubaneswar, Odisha, India
Abstract
Gestational diabetes mellitus (GDM) refers to a condition characterized by varying degrees of glucose intolerance, which is initially identified during pregnancy. It is typically identified by conducting screenings on pregnant women to assess their clinical risk factors. Subsequently, among those deemed at risk, diagnostic tests are performed to evaluate their glucose tolerance. It is worth noting that women diagnosed with these diseases face an elevated likelihood of experiencing or developing diabetes outside of the pregnancy period. It refers to the occurrence of elevated blood glucose levels during pregnancy. The disease includes hyperglycaemia of varying degrees, ranging from pre-existing type 2 diabetes diagnosed during pregnancy to the development of full-blown GDM during pregnancy. It is associated with various adverse outcomes for both the mother and the new-born. These include increased birth weight and increased C-peptide levels in cord blood serum. In addition, having gestational diabetes puts you at a higher risk of developing diabetes in the future. The study's most important findings on awareness primarily affected respondents from cities -76.59%, in semi-urban areas it was 67.77% and in rural areas it was lowest -23.54%. The perception results show that the majority of respondents believe that AI has transformed healthcare services with lower costs and greater accuracy while providing other benefits.
Graphical Abstract
Keywords
Main Subjects
Introduction
Gestational diabetes mellitus (GDM) is a condition characterized by varying degrees of glucose intolerance that occurs or is first recognized during pregnancy. It is widely acknowledged as one of the most prevalent clinical complications associated with pregnancy [1,2]. Based on the findings of the International Diabetes Federation (IDF) in 2017, it is anticipated that the incidence of GDM will exhibit an upward trend over successive years [3]. It has been observed that women diagnosed with GDM may be susceptible to experiencing unfavorable consequences [4,5]. Mothers diagnosed with GDM face an increased likelihood of developing gestational hypertension and preeclampsia, as well as a higher risk of undergoing a cesarean section. In addition, they are at a heightened risk of developing subsequent type 2 diabetes mellitus (T2DM) and cardiovascular diseases, as supported by previous studies [6-11]. Infants born to women with GDM may exhibit an increased susceptibility to abnormal fetal development. It includes the occurrence of macrosomia, a condition characterized by excessive birth weight, a higher likelihood of congenital abnormalities [6,12-13]. Therefore, it is recommended that healthcare policymakers maintain a keen awareness of the importance of GDM in terms of its implications for early identification and subsequent intervention.
To date, a multitude of pertinent factors have been identified as predictors of this disease. Numerous studies have provided evidence supporting the association between gestational diabetes and GDM, and various risk factors. These commonly reported risk factors include advanced maternal age, pre-pregnancy obesity. A family history of diabetes (FHD), previous adverse obstetric outcomes such as macrosomia, stillbirth, abortion, premature delivery, congenital anomalies, being a primi-gravida, The history of GDM, infection factors such as Human Immunodeficiency Virus (HIV), smoking, and socio-economic factors such as educational level, occupation, and monthly household income.
Among the available polymorphisms, only the 5'UTR c.331 G>A is related to breast cancer in mastectomies and lumpectomies women [31-32]. Diabetes is a biological problem of life in a new way in human societies, especially in developing countries. Environmental and genetic factors are mutually influential in the incidence and exacerbation of this disease [32-33].
Artificial intelligence (AI) presents substantial prospects for advancement and innovation, as it effectively addresses cognitive challenges that traditionally necessitate human intelligence. Voice recognition, recommendation systems, and self-driving cars exemplify the tangible achievements of AI across diverse fields. Probably, forthcoming advancements in the field of AI will yield even more substantial outcomes. According to a report by the International Data Corporation (IDC) [25].
it is projected that expenditure on AI will witness substantial growth, reaching an estimated value of 97.9 billion by 2023. The potential of AI in enhancing individuals' health and well-being is considerable, owing to the growing availability of electronic health records (EHRs) and other patient-related data. AI can augment clinicians' diagnostic processes, identify opportunities for prevention, and provide personalized treatment recommendations, among various other applications. Despite the existence of a few rudimentary assistive tools that have been implemented in practical settings [26-27].
The advent of AI has brought about a gradual transformation in the field of medical practice. The AI utilization in the medical domain has led to the development of numerous applications that find utility across various medical disciplines, including clinical, diagnostic, rehabilitative, surgical, and predictive practices. The field of medicine is witnessing significant advancements in clinical decision-making and disease diagnosis due to the integration of AI technologies. AI technologies can process and examine extensive amounts of data from various sources to identify diseases and provide guidance for clinical decision-making [28-29].
Role of AI in health care
This can increase healthcare productivity and efficiency, enabling healthcare systems to provide more and better care to more people. Artificial intelligence can help improve the experience of healthcare workers, allowing them to spend more time on direct patient care and reduce burnout. Artificial intelligence offers the opportunity to reduce human errors, support professionals and medical staff, and provide patient care around the clock. As AI tools advance, AI can be used even more widely to read medical images, x-rays and scans, diagnose medical problems, and plans.
Objectives of the study
- To study the awareness level of GDM among pregnant women in the urban, rural, and semi-urban areas of the Mumbai region.
- To know the opinion of healthcare practitioners such as nursing, house surgeon, and assistant professors towards AI's role in GDM.
Sample size determination for unknown populations
N= Z2 (P) (1-P)/ C2 = (1.96)2(0.5) (1-0.5)/ (0.05)2 = 384
Where, Z= Standard normal deviation set at 95% confidence level is 1.96, P= Percentage picking choice or response is 0.5, and the C= Confidence interval is 0.05
To gather the necessary data, a combination of cluster and random sampling methods was employed. A total of 783 individuals were initially approached for participation. However, after careful evaluation, it was determined that 387 respondents provided valid and complete responses, meeting the criteria for inclusion in the final dataset. To achieve a more comprehensive and accurate representation, all of the responses were included in the analysis. The study sample comprised 143 individuals who were pregnant at the time of data collection, while the remaining participants were identified as healthcare practitioners.
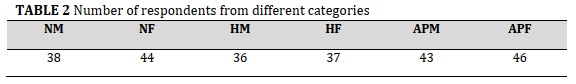
Here, NM stands for Nursing male, NF- Nursing female, HM- House surgeon male, HF- House surgeon female, APM- Assistant Professor Male, APF- Assistant Professor Female
According to Table 2, 38 were male nursing staff, 44 were female nursing staff, 36 were male house surgeons, 37 were female house surgeons, 43 were male assistant professors, and the rest were female assistant professors.
Research Design
Both primary and secondary data are used in this study. Pregnant women, nursing staff, house surgeons, and doctors of assistant professor level were considered as primary data. The total period is spread over six months. The variables were mostly derived from core group discussions and some were from the review of the literature. In this regard, eight core group discussions were made consisting of pregnant women, doctors, and nursing staff of various super specialty hospitals in study areas. Initially, more than 24 attributes were identified, however, after continuous deliberations with various groups, the attributes were finally restricted to 17 only. A simple weighted perception score method was used for the various sub-variables considered for the study. A 5-point Rensis Likert scale was used to measure each attribute. Weights of 5 for completely agreeing on responses, weights of 4 for agreeing on responses, weights of 3 for neutral stands, weights of 2 assigned for disagreeing responses, and weights of 1 assigned to completely disagreeing responses. Cluster and snowball sampling method used to collect the perceptions of the health care service providers and for the awareness level random sample being used. For confidentiality, the names of the hospitals were not disclosed.
Table 1, shows that in the urban areas, 56 respondents participated, in rural areas 42 respondents participated and the rest were from semi-urban areas.

Table 2, shows the various categories of respondents related to nursing, house surgeon and assistant professors.
Scope of the study
The present scope of the study includes various urban, rural, and semi-urban areas of Mumbai. The sample includes from the pregnant women associated with advertising sector. The pregnant women in advertising sector have to sit before the computers for long hours which leads to obesity& stress culminating in smoking which in turn spikes the blood glucose levels during pregnancy leading to GDM. The justification being, during the interaction with health care practitioners it was observed that this is one segment on whom not much study has been undertaken. The participants include male and female nursing staff, male and female house surgeons, and male and female assistant professors.
Various localities of urban, rural and semi-urban is mentioned in the Table 3.
In Figure 1, the awareness level of GDM in urban pregnant women was 59.63%, 12.96% in rural areas, and 36.17% in semi-urban areas. For the partial awareness level among pregnant women in urban areas 16.96%, 10.58% in rural areas, and the same for the semi-urban areas 31.60%. Similarly, 76.46% of rural areas pregnant women were not aware of GDM, 32.03% in semi-urban not aware of GDM, and 23.41% in urban areas.

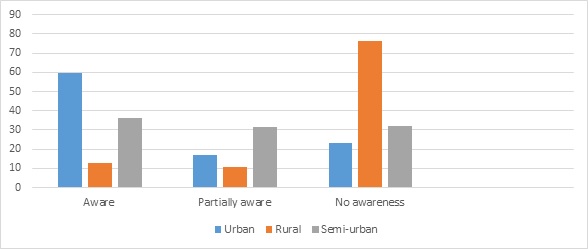
FIGURE 1 Awareness level of GDM
Source: Annexures 1,2, and 3
The Maximum Possible Weight = responses X Variables X maximum weight
In Table 4, the maximum possible weight and least possible weight were ascertained for various health care practitioners. The weight scores were used in Table 5- perception of health care practitioners.

Figure 2, shows the perception weight of nursing male and female, weight of house ssurgeon male and female and for the assistant professor male and female.
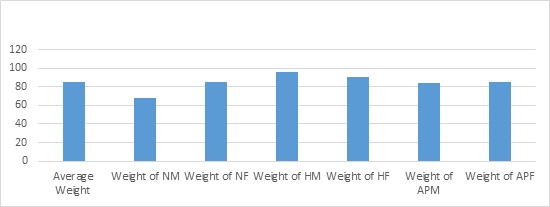
FIGURE 2 Represents weight of different respondent groups
Data interpretation
With reference to Table 5, The total weight of various health care practitioners such as NM, NF, HM, HF, APM, and APF were 2208, 3193,2924, 2861, 3077, and 3334 respectively. This shows that the percentage of actual total weight to maximum possible weight was 68.40%, 85.37%, 95.55%, 90.97%, 84.19%, and 85.27%. The average % was 84.96%. This indicates that even though the majority of participants have positive opinions, however, in the case of nursing males have less perception. This may be due to they were not equipped with the AI technology or may have less awareness about its benefits. The opinion may differ when we take a different set of populations. The 84.96% signifies all the attributes considered for the present study having relevant for the current study.


Results
Related to awareness level, in the urban areas the awareness level among the respondents around 76.59% and the unaware level were 23.4%. For the rural segment 76.46% were not aware and rest were aware. There was a huge gap in the awareness level. Similarly, for the semi-urban areas the awareness level of fully and partially comes to 67.77% only.
As far as perceptions for the various attributes by different respondents, the perception level of HM were highest with 95.55% of maximum possible weight followed by the HF approximately 90.97%. At the same time for the NF and APF were more than 85%, similarly others also having significant opinion base for the various attributes considered AI’s relevance to the health care services as per the opinion of the various respondents.
Implications of the study
- More awareness among the pregnant women needs to be initiated more specifically in rural and semi-urban areas.
- Educate the AI biases to the staff and patients.
- Data security measures should be strengthened.
- Transparency can be enhanced on customised basis.
 Figure 3, shows the the impact of gestational diabetes.
Figure 3, shows the the impact of gestational diabetes.
Conclusion
Gestational Diabetes Mellitus (GDS) is one of the challenges that healthcare practitioners face in recent times. However, through technological advancement, there are a lot of transformations in healthcare services. More specifically, the AI plays a crucial role in our life. This facilitates the GDM patients, risk assessment, accuracy in diagnosis, enhanced health care, and reduction in human error in addition to others. In this study, it was observed that there is a need for more awareness level of GMD affect in rural areas and sub-urban areas for the women working in the advertisement sector.
The male nursing staff and others who are not involving themselves in the adoption of AI technology should be encouraged to learn the same. This will provide an added advantage to the health care service. To conclude the findings, it was observed that house surgeon male female considers AI having more beneficial followed by assistant professor staff and nursing staffs.
Data inclusion and exclusion criteria
The participants in this study consisted exclusively of pregnant women, nursing staff, house surgeons, and assistant professors in the medical field. These individuals were selected based on their willingness to volunteer and their agreement to take part in data collection activities. The task of classifying the exclusion and inclusion criteria proved to be highly demanding, yet the diligent researchers successfully gathered the intended sample size.
Acknowledgments
The authors express their gratitude to all the participants comprising the nursing and house surgeon staff from various hospitals also the pregnant women of the advertising sector from a different demography. The invaluable feedback and active engagement of the participants greatly contributed to the successful completion of the current study.
Conflict of interest
The current study represents the collaborative efforts of the authors, who affirm that they do not possess any conflicts of interest with regard to any involved individuals or institutions. At present, no financial resources have been procured for the ongoing investigation.
Orcid
Bhole Nath Thakur: https://www.orcid.org/0009-0004-0053-3525
Ipseeta Satpathy: https://www.orcid.org/0000-0002-0155-5548
Patnaik, B.Chandra Mohan*: https://www.orcid.org/0000-0002-7927-0989
Abhishek Kumar: https://www.orcid.org/0000-0002-0876-3219
-----------------------------------------------------------------------
How to cite this article: Bhole Nath Thakur, Ipseeta Satpathy, B.Chandra Mohan Patnaik *, Abhishek Kumar, Artificial intelligence (AI): transformation in gestational diabetes mellitus (GDM) treatment in india. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(4), 456-465. Link: http://jmpcr.samipubco.com/article_186165.html
-----------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.