Document Type : Original Research Article
Authors
Department of Radiodiagnosis, Saveetha Institute of Medical and Technical Sciences, Thandalam, Tamil Nadu, India
Abstract
Introduction: This study assesses the role of ultrasound elastography in distinguishing between malignant and benign focal liver lesions (FLLs), a crucial challenge in gastroenterology.
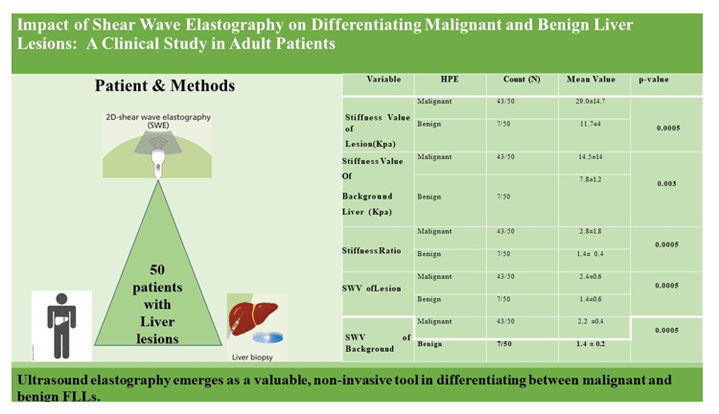
Methodology: Executed in a tertiary care hospital in South India, the research included 50 subjects, predominantly male. The inclusion criteria were patients with FLLs identified via ultrasound, excluding lactating or pregnant women and individuals with previously treated lesions. Shear wave elastography (SWE) was the primary used method, with independent sample t-tests and Chi-Square tests for statistical analysis of elastographic parameters.
Results: Among the lesions, 78% were malignant. Notable differences were observed in stiffness value, stiffness ratio, and shear wave velocity (SWV), with a stiffness cut-off of 16.4 kPa indicating 79.10% sensitivity and 85.70% specificity.
Discussion: The study's findings align with existing literature, underscoring the utility of SWE in differentiating lesion types. This reinforces the elastography value in clinical diagnostics, especially in accurately categorizing liver lesions, thereby guiding appropriate medical interventions.
Conclusion: Ultrasound elastography, specifically through SWE, demonstrates significant effectiveness in distinguishing between malignant and benign FLLs, offering a promising tool for accurate clinical diagnosis. Future studies with diverse patient groups and lesion types are essential to expand the utility and applicability of this diagnostic technique.
Graphical Abstract
Keywords
Main Subjects
Introduction
Liver diseases, a long-standing global health concern, have gained prominence due to their widespread prevalence and inadequacy of traditional diagnostic methods. Focal liver lesions (FLLs), encompassing both solid and cystic abnormalities in the liver, have become increasingly detectable with advances in imaging technologies. The management of these lesions, crucial in both benign and malignant cases, significantly impacts healthcare expenses and patient care strategies. Imaging plays a pivotal role in the evaluation of FLLs, starting with conventional ultrasonography (US) enhanced by Color-Doppler and Contrast Enhanced Ultrasound (CEUS) for initial assessments. There have been numerous studies pertaining to diagnosis of hepatic lesions using advanced imaging modalities. While magnetic resonance imaging (MRI) and computed tomography (CT) offer detailed analysis, they are more expensive and less accessible. Contrast-enhanced imaging provides high diagnostic accuracy, but often necessitates confirmatory invasive biopsies [1,2].
This study focuses on ultrasound elastography, a non-invasive, efficient technique for identifying liver lesions. The objective of this study is to gather and analyse elastographic parameters (stiffness value, stiffness ratio, and shear wave velocity), correlating them with histopathological findings to differentiate between malignant and benign liver tumors, thereby assessing the method's diagnostic efficacy. This study could thereby address these lesions using minimal intervention and less expense to the patient.
Experimental
Materials and methods
This study, conducted at a tertiary level teaching hospital, over 18 months (September 2020 – March 2022), is a prospective analysis involving 50 patients. It focuses on individuals aged 20 to 80 years, of both sexes, presenting with focal liver lesions identified through ultrasound (USG), conventional CT, or MRI. Excluded were lactating or pregnant females, patients with previously treated liver lesions, those with gross ascites, simple hepatic cysts, and uncooperative patients.
After obtaining clearance from the Institutional Ethics Committee and adhering to informed consent guidelines, patients referred for image-guided biopsy or scheduled for surgical resection of liver lesions were included. Participants were selected based on defined inclusion and exclusion criteria, and relevant data were gathered from their medical records.
Elastographic examinations were conducted using a 3.5MHz convex probe on a PHILIPS AFFINITI 70G ultrasound system. The process involved positioning patients to optimize the acoustic window, focusing on the largest lesion or the background liver for measurement. Shear Wave Elastography (SWE) was performed, with liver stiffness measured in two specific areas. Stiffness value (kPa), stiffness ratio, and shear wave velocity (m/s) were recorded, averaging five measurements per patient for analysis.
For statistical analysis, IBM SPSS Statistics for Windows, Version 23.0, was employed. Descriptive statistics like frequency and percentage analyses were used for categorical variables, while mean and standard deviation were applied to continuous variables. The Independent sample t-test assessed differences between bivariate samples in independent groups. Chi-Square test was used for qualitative categorical data, and Fisher's Exact test for 2×2 tables with expected cell frequencies less than 5. A p-value of 0.05 was considered significant in these statistical evaluations.
Results
In this study involving 50 focal liver lesions, 78% (39 lesions) were malignant, with metastases (53.8%) (Figure 1), hepatocellular carcinoma (HCC, 38.5%), and cholangiocarcinoma (7.7%) being the primary types. The remaining 22% (11 lesions) were benign (Figure 2), all identified as hemangiomas (Table1). The mean elastographic parameter such as stiffness value, stiffness ratio, and shear wave velocity are presented in Table 2.
The study's demographic breakdown showed a varied age distribution with a mean age of 57.10±13.30 years and a male predominance (74%). Histopathological Examination (HPE) reports revealed distributions of cholangiocarcinoma (6%), HCC (30%), hemangioma (22%), and metastasis (42%) (Table 1).
Statistical analysis revealed few significant findings. Age showed a strong correlation with HPE types (p=0.002), while sex, lesion number, vascularity, background liver condition, and portal vein involvement did not show statistical significance with HPE (Table 3). Notably, elastographic parameters such as lesion stiffness value, background liver stiffness, stiffness ratio, and shear wave velocity (SWV) of the lesion as well as background demonstrated high statistical significance with HPE (p<0.01) (Table 2).
Receiver Operating Characteristic (ROC) curve analysis further validated these findings. The area under the curve (AUC) for the stiffness value of the lesion was 0.889 (p=0.001), indicating high sensitivity (79.1%) and specificity (85.7%) at a cutoff of 16.4. The stiffness ratio's AUC was 0.723, showing lower sensitivity (62.8%) and specificity (71.4%) with no statistical significance (p=0.061). However, the SWV of the lesion's AUC was 0.922 (p=0.0004), displaying high sensitivity (83.7%) and specificity (85.7%), indicating the overall accuracy of the test in differentiating lesion types (Table 4). These results underscore the efficacy of elastography in assessing focal liver lesions, with significant implications for clinical diagnostics.
Discussion
This study aimed to analyse the capabilities of ultrasound elastography in distinguishing between benign and malignant focal liver lesions (FLLs), a prevalent diagnostic challenge in the field of gastroenterology. Among the 50 subjects, the individuals were primarily male, with a notable age disparity observed between those diagnosed with malignant lesions, averaging 62 years, and those with benign lesions, averaging 38 years. A significant finding of the study was that a majority of the lesions, about 78%, were malignant. This highlights the critical need for precise and reliable diagnostic tools in the assessment of liver pathology.
In terms of classification, FLLs encompass a range of lesions, including haemangiomas, which are typically benign and identifiable through specific imaging patterns on ultrasound (USG) and magnetic resonance imaging (MRI). Other benign lesions such as focal nodular hyperplasia (FNH) and hepatic adenomas also display distinct characteristics visible on USG, CT, and MRI. On the other hand, malignant FLLs, like metastasis, intrahepatic cholangiocarcinoma, and hepatocellular carcinoma, are each characterized by unique risk factors and imaging profiles, making accurate diagnosis crucial for effective treatment [3,4].
The use of ultrasound elastography, particularly sensitive to variations in tissue stiffness, has become increasingly pivotal in medical imaging. This study primarily employed shear wave elastography (SWE) for quantitative measurement of tissue elasticity. This advanced imaging technique categorizes various parameters into qualitative, semi-quantitative, and quantitative groups, providing a comprehensive analysis of the lesion characteristics. Despite its significant utility in clinical practice, ultrasound elastography is not without limitations. One of the primary constraints is its operator dependency, which can lead to variability in measurements. This variability often stems from differences in tissue composition or the presence of pathologic processes within the tissues being examined [5-8].
The effectiveness of ultrasound elastography in differentiating benign from malignant liver lesions is corroborated by several studies cited in this research. Notably, the works of Park et al. [9], Gallotti et al.[10], and Guo et al. [11] have reported considerable differences in shear wave velocity (SWV) values between these two types of lesions. These findings suggest that malignant lesions typically exhibit higher SWV values compared to benign ones, a distinction that can be crucial for accurate diagnosis. In contrast, studies by Ronot et al. [12] and Choi et al. [13] found no significant differences in mean stiffness values between benign and malignant lesions, suggesting the FLLs complexity and diversity. Supporting these results, Shuang-Ming et al. [14] and Yu and Wilson et al. [15] also identified significant differences in acoustic radiation force impulse values, further emphasizing the diagnostic potential of ultrasound elastography in liver lesion assessment.
Our study's results align with these findings, with notable differences observed in stiffness value, stiffness ratio, and SWV between malignant and benign lesions. For instance, a cut-off value for stiffness was identified at 16.4 kPa, yielding a sensitivity of 79.10% and specificity of 85.70% (Figure 1). These findings are in line with Li et al.'s study [16], which reported higher stiffness values in malignant tumors. However, contrasting these results, Heide et al. [17] found similar stiffness values between benign and malignant tumors, highlighting the potential variability of elastographic properties in these lesions. In addition, our study resonates with Yu et al.'s findings, which indicated significant differences in stiffness values between benign and malignant lesions (Figure 2).
Malignant liver lesions generally exhibit higher SWV values than benign ones, allowing for effective differentiation. SWV cut-off values, varying for different lesion types, enhance diagnostic accuracy. The variability in SWV values across studies highlights the potential of elastography in characterizing liver lesions, although results can differ based on the lesion type and study conditions [18,19].
However, the study is not without limitations. The small sample size of benign lesions, comprising only 11 haemangiomas, limits the generalizability of the results. The research, being conducted in a single centre, may also have restricted the broader applicability of its findings. Other limitations, such as the unaddressed impact of transducer distance on stiffness assessment and the absence of interobserver variability documentation, were noted. The operator-dependent nature of sono-elastography and challenges in patient compliance during exams were additional constraints observed in the study.
Conclusion
Ultrasound elastography emerges as a valuable, non-invasive tool in differentiating between malignant and benign FLLs. By quantifying lesions' mechanical properties, it offers a nuanced approach to liver lesion diagnostics, supplementing traditional ultrasound techniques. Despite its promising results, our study highlights the need for broader, multi-centre research to enhance the validity and applicability of elastography in clinical settings. As Sono-elastography continues to evolve, it holds potential for more refined and targeted diagnostic strategies in liver pathology.
ORCID
Vishnu Raj: https://www.orcid.org/0009-0004-2436-4586
Arunkumar Mohanakrishnan: https://www.orcid.org/0009-0002-0376-5001
Iffath Misbah*: https://www.orcid.org/0009-0005-4018-3686
Paarthipan Natarajan: https://www.orcid.org/0000-0002-8972-5969
-----------------------------------------------------------------------------------------
How to cite this article: Vishnu Raj, Arunkumar Mohanakrishnan, Iffath Misbah*, Paarthipan Natarajan, Impact of shear wave elastography on differentiating malignant and benign liver lesions: a clinical study in adult patients. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(5), 603-608. Link: http://jmpcr.samipubco.com/article_187284.html
-----------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.