Document Type : Review Article
Authors
- Mansour Deylami 1
- Majid Vatankhah 2
- Tayyebeh Zarei 2
- Ehsan Rahmanian 3
- Farshid Javdani 3
- Shahram Shafa 3
- Hasan Zabetian 3
- Minou Najar Nobari 4
- Kaveh Hedayati Emami 5
- Fatemeh Maleki 6
- Amin Shafiei 3
- Vida Hafezi 7
- Roohie Farzaneh 8
- Mohammad Sadegh Sanie Jahromi 3
1 Assistant Professor of Anesthesiology, Department of Anesthesiology and Critical Care, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran
2 Anesthesiology, Critical Care and Management Research Center, Hormozgan University of Medical Sciences, Bandar Abbas, Iran Pain
3 Research Center for Social Determinants of Health, Jahrom University of Medical Sciences, Jahrom, Iran
4 Orofacial Pain and Dysfunction and Sleep Disorders Department, School of Dentistry, UCLA, Los Angeles, California, US
5 Department of Anesthesiology and Critical Care, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran
6 Department of Emergency Medicine, Faculty of Medicine, Birjand University of Medical Sciences, Birjand, Iran
7 Student Research Committee, Alborz University of Medical Sciences, Alborz, Iran
8 Department of Emergency Medicine, Faculty of Medicine, Mashhad University of Medical sciences, Mashhad, Iran
Abstract
The concern has recently been raised for disease status and management of people with narcolepsy after initiation of COVID-19 pandemic. Here, we evaluated the literature to determine how the COVID-19 pandemic has impacted the lives of narcolepsy patients. This was a systematic review and meta-analysis study on online databases of Web of Science, PubMed, Scopus, and ScienceDirect using keywords of “Narcolepsy”, “Sleepiness “, “cataplexy”, “nightmare”, “nocturnal sleep”, “COVID-19”, “Pandemic”, “SARS-COV2”, and “Coronavirus”, looking for observational studies. Statistical analyses were performed by CAM software with significance level being considered at under 0.05 as statistically significant. Total number of 9 studies were included with 607 patients with narcolepsy. With a heterogeneity of 99.94%, pooled mean differences (MD) of Epworth Sleepiness Scale (ESS) scores before and after the pandemic/lockdowns was -1.54 (95%CI: -1.55 to -1.53, P<0.01). The most prevalently increased symptom among the narcolepsy patients was naps taken during the day (58.81%, 95%CI of 50.85 to 66.34) followed by the increased appetite (45.15%, 95%CI of 28.91 to 62.49). Our study shows that disease status of narcolepsy patients is affected by COVID-19 pandemic. We can assist narcolepsy patients in this challenging position by being aware of their unique demands during the COVID-19 illness and sympathetic to their sensitivity.
Graphical Abstract
Keywords
Main Subjects
Introduction
Narcolepsy is a neurological disorder that affects the control of sleep and wakefulness [1]. Individuals affected by narcolepsy experience daytime sleepiness and intermittent, uncontrollable periods of sleeping during the day. These sudden attacks of sleep may occur during any type of activity and at any time of the day [2]. Drowsiness during the day has led to mistakes and sometimes human accidents and tragedies in industrial societies, and variable statistics have been reported in terms of accidents and deaths caused by narcolepsy [3]. Narcolepsy management by medications is also one of the other ways to treat sleep attacks, which is used in some people with severe and damaging symptoms of this disorder [4]. Some drugs, such as those in the stimulant group as well as the Modafinil, Methylphenidate, and amphetamines are mainly used to treat this sleep disorder [4]. Human life has faced serious challenges with spread of the COVID-19 pandemic [5]. People were advised to stay at home, required to use personal protective equipment, and many countries' economies suffered a recession [6] . Most medical emergencies have experienced interruptions in standard care; this affected the regularity of providing care for other diseases than COVID-19 [7]. Quarantine measures led to changes in bedtime and waking-up schedules, contributing to circadian misalignment for narcolepsy patients [8]. COVID-19 lockdowns affected the sleep quality and daytime condition of narcolepsy patients, emphasizing the broader impact on well-being [9]. Some narcolepsy patients faced job loss, leading to altered working/studying conditions and potential lifestyle shifts [10]. Effects of the COVID-19 pandemic’s quarantines and restrictive roles has been well studied on both acute [7,11]. and chronic diseases [12].Recently, some studies have focused on the same issue for the narcolepsy patients. Here, we conducted a systematic review of the literature to determine how the COVID-19 pandemic affected narcoleptic patients’ lives. By knowing about the special needs of narcolepsy patients during the COVID-19 disease and being sensitive to their vulnerability, we can help them in this difficult situation. The objective of this study was to compare clinical status of narcoleptic patients, before and after COVID-19.
Methods
We conducted a systematic review and meta-analysis from July to November, 2022 based on the PRISMA statement. The objective of this study was to examine the effect of COVID-19 pandemic on narcolepsy patients.
Search strategy
The required information has been collected in online databases of Web of Science, PubMed, Scopus, and ScienceDirect using keywords of “Narcolepsy”, “Sleepiness “, “cataplexy”, “nightmare”, “nocturnal sleep”, “COVID-19”, “Pandemic”, “SARS-COV2”, and “Coronavirus”. The period selected for searching articles was from 2019 to 2022. To identify and cover more published articles, after searching the databases, several authoritative journals in this field were also searched manually. Reference lists of full text eligible papers were also manually searched for potentially relevant papers. All search steps were performed independently by two authors.
Eligibility
The inclusion criteria included studies reporting indices of hypersomnia before pandemic compared with during the pandemic in patients with narcolepsy of any type. Likewise, studies reporting these indices before and during a lockdown and quarantine were included. We did not impose any limitations on age or study area and only included English language papers. The exclusion criteria comprised of interventional studies, articles presented in conferences, case reports, letters to the editor, and non-peer reviewed sources. Two independent evaluators performed eligibility assessments and a third researcher judged any disagreement in selection of studies.
Data extraction
All articles were evaluated by two evaluators using a checklist after extracting them from the desired reports. To extract data, a data extraction form was designed manually in the Excel software environment, and the extracted information in this form included: author's name, year of publication of the article, name of the country, characteristics and number of participants, the methods of assessment of narcolepsy, reported changes in symptoms, and numerical objective assessments of the narcolepsy before and after lockdowns. Variables of Epworth Sleepiness Scale (ESS), frequency of cataplexy, appetite changes, disturbed nocturnal sleep, naps taken per day, nightmares, and sleep attacks were extracted for meta-analyses.
Quality assessment
Joanna Briggs Institute (JBI) tool was used for critical appraisal of the papers with retrospective study design. This included 8 questions about the different methodological aspects of the study. Studies with less than 5 forgathered criteria were considered as low quality. Based on the mentioned criteria, there should be clear and well-defined inclusion criteria outlining participant characteristics, study design, and relevant interventions. In addition, the subjects and settings should be clearly described. Valid and reliable exposure and outcome measures as well as employing standard methodologies are essential to ensure the accuracy of collected data. The identification of potential confounding factors and the implementation of strategies to address them, such as matching or statistical adjustments, demonstrate a robust study design. Ultimately, the use of appropriate statistical methods and transparent reporting contributes to the overall appraisal of study quality, ensuring the validity and reliability of the findings in the context of the research synthesis.
Statistical analysis
The effect size was flexibly selected based on the reported outcomes in included studies. Qualitative measures were pooled in form of event rates in one group. Event rates of subjective changes in symptoms of narcolepsy before and after lockdowns were used in calculations. In case of quantitative data, where data of before and after lockdown were provided, differences in means were pooled by random model effect size. P-value of under 0.05 was considered as statistically significant. To perform meta-analysis, CMA 3 (Comprehensive Meta-Analysis) software was used. I2 above 50% was considered as heterogeneous in study based on the Q statistic.
Results
After removing the articles that were weakly related to the objectives of the study and selecting the original articles, the list of sources of the selected articles was also searched to increase the certainty of identifying and reviewing the existing articles.
Total number of 9 studies was included in our review as listed in Table 1. Total number of 607 patients with narcolepsy was evaluated. ESS changes were compared before and after pandemic/lockdown in 4 studies. Other studies had only reported ESS measures to address the severity of disease.
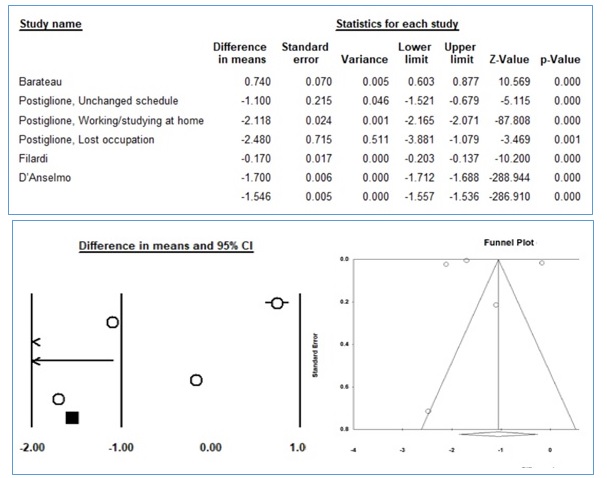
Pooling the mean differences (MD) of Epworth Sleepiness Scale (ESS) scores before and after the pandemic, 4 studies were included in which Postiglione et al. study had expressed their results based on the 3 different groups of patients, that we defined each of them as an independent sample for pooling. Finally, with a heterogeneity of 99.94%, pooled MD was -1.54 (95%CI: -1.55 to -1.53, P<0.01), as displayed in Figure 1. Funnel plot in Figure 1 (right side), does not show evidence of asymmetry. Egger’s test revealed no publication bias (P=0.472).
In forest plot (left), the size of each circle represents the sample size and the lines drawn on each side of the square represent the 95% confidence interval for each study; Funnel plot (right side) shows the symmetric distribution of log differences in mean based on the standard errors. We pooled event rate of self-reported increase in symptoms of narcolepsy under random effect size for the studies with high heterogenicity (>75%) and fixed effect size for the rest. The most prevalently increased symptom among the narcolepsy patients was naps taken during the day (58.81%, 95%CI of 50.85 to 66.34) followed by the increased appetite (45.15%, 95%CI of 28.91 to 62.49). Other symptoms were less frequently increased, as well as the disturbed nocturnal sleep, nightmares, frequency of cataplexy, as presented in Table 2. No publication bias assessment was performed as epidemiologic proportional data does not require.
Quality assessment
As indicated in Table 3, inclusion criteria were clear in all studies and patients with narcolepsy based on the ICSD-3; International classification of sleep disorders-third edition had been selected. Except for the Zhao study, all studies had clear settings, periods of study, and subjects. Exposure that was lockdown or pandemic effects were not well demonstrated in most studies and only Aguilar et al., Postiglione et al., and Zhao et al. studies evaluated effects of lockdowns on working/studying schedules. Confounding factors were identified in most circumstances but adjustments for decreasing their negative consequences were not performed in studies.
Discussion
We conducted a systematic review and meta-analysis of effects of COVID-19 pandemic on clinical conditions of narcoleptic patients. Our study showed that Epworth Sleepiness Scale (ESS) scores in narcolepsy patients has significantly decreased after the initiation of pandemic or lockdowns (-1.54 , 95%CI: -1.55 to -1.53; P<0.01). In addition, the data showed that number of naps taken during the day increased significantly. These two findings are consistent with the known effects of daytime naps on reducing sleepiness in narcoleptic patients. Furthermore, the nighttime symptoms of narcolepsy did not differ with the pandemic. As we know that when subjective sleepiness, assessed by ESS, is higher than 10, daytime sleepiness is high. However, deciding that if 1.54 points decrease in ESS is also clinically significant is a bit complex. In this case, we also should consider the qualitative conclusions of studies. Most studies have mentioned deteriorated measures of the day time sleepiness in narcolepsy following the lockdowns [10, 13-14]. while reports of improvement in subjective sleepiness struggled along [15,16]. Zhao et al. attributed this improvement in daytime symptoms of narcolepsy to increased total sleep time (TST) in lockdown period. Laclause et al. reported various transformations in the time metrics of daytime and night time sleep of NT patients that its interpretation was not comprehensively provided [17]. Therefore, it seems that COVID-19 is affecting sleep quality and day time wakefulness in narcolepsy patients but the direction of the effects is widely distinct in different individuals. Our study findings also justify the finding of decreased day time sleepiness as daytime naps have been being scheduled in treatment process of the narcolepsy patients [18]. However, in patients who their clinical status does not respond to stimulant medications, naps are not recommended [19]. This might be a huge source of heterogenicity in combining data of included studies as we were not able to pool data of variations in adherence to medications during the COVID-19 pandemic. The most prevalently increased symptom among the narcolepsy patients was naps taken during the day (58.81%, 95%CI of 50.85 to 66.34) followed by the increased appetite (45.15%, 95%CI of 28.91 to 62.49). Increased BMI in narcolepsy patients has been previously studied and cited to be more prevalent than general population [20]. and has been known as a linked disease to narcolepsy [21].
COVID-19 is directly been associated with narcolepsy, based on the SARS-COV2 infected case reports that have experienced excessive daytime sleepiness [22]. The biomolecular mechanisms of such interaction was explained for Influenza virus [23]. But, beyond the pathophysiological investigations, participants with previously diagnosed narcolepsy are known as a population with special care needs and their disease status during the COVID-19 pandemic has been evaluated by some studies that we seek to review.
This study has some limitations in this study. While we used a comprehensive systematic review strategy, there might be studies that were missed by our literature review. In addition, response rate to surveys in some studies were low (26.5% in [24]; 40.71% in [13]. Furthermore, there are various confounding factors that are not controlled in our study, as well as the age, gender, ethnicity [25]., or other known and unknown ones.
Conflict of Interest
The authors have no conflict of interest to declare.
Funding Statement
This research did not receive any specific grant from funding agencies in the public.
Ethical approval
There is no ethical issue.
Acknowledgments
The authors would like to thank the Clinical Research Development Unit of Peymanieh Educational and Research and Therapeutic Center of Jahrom University of Medical Sciences for providing facilities to this work
Orcid:
Mansour Deylami*: https://www.orcid.org/0000-0002-5933-3219
Majid Vatankhah: https://www.orcid.org/0000-0002-2053-1138
Tayyebeh Zarei: https://www.orcid.org/0000-0001-8605-7742
Ehsan Rahmanian: https://www.orcid.org/0000-0002-1321-8688
Farshid Javdani: https://www.orcid.org/0000-0002-7850-3519
Shahram Shafa: https://www.orcid.org/0000-0001-9888-4630
Hasan Zabetian: https://www.orcid.org/0000-0002-2507-4431
Minou Najar Nobari: https://www.orcid.org/ 0009-0000-3010-3543
Kaveh Hedayati Emami: https://orcid.org/0000-0001-5920-396X
Fateme Maleki: https://www.orcid.org/0000-0002-6823-5151
Amin Shafiei: https://www.orcid.org/ 0000-0003-0005-4319
Vida Hafezi: https://www.orcid.org/ 0009-0005-4287-881X
Farzaneh Roohie: https://www.orcid.org/0000-0002-0892-1555
Mohammad Sadegh Sanie Jahromi: https://www.orcid.org/0000-0001-8437-1092
------------------------------------------------------------------------------------------------
How to cite this article: Mansour Deylami*, Majid Vatankhah, Tayyebeh Zarei, Ehsan Rahmanian, Farshid Javdani, Shahram Shafa, Hasan Zabetian, Minou Najar Nobari, Kaveh Hedayati Emami, Fateme Maleki, Amin Shafiei, Vida Hafezi, Farzaneh Roohie, Mohammad Sadegh Sanie Jahromi, Systematic review and meta-analysis of narcolepsy management during the covid-19 pandemic. Journal of Medicinal and Pharmaceutical Chemistry Research, 2024, 6(3), 292-301. Link: http://jmpcr.samipubco.com/article_184365.html
------------------------------------------------------------------------------------------------
Copyright © 2024 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
.png)
.png)
.png)
